
This article is about the most common aging brain problem that you may have never heard of.
While leading a fall prevention workshop a few years ago, I mentioned that an older person’s walking and balance problems might well be related to the presence of “small vessel ischemic changes” in the brain, which are very common in aging adults. (This is also called “white matter disease.”)
This led to an immediate flurry of follow-up questions. What exactly are these changes, people wanted to know. Do they happen to every older adult? Is this the same as vascular dementia? And how they can best help their parents with cognitive decline?
Well, these types of brain lesions don’t happen to every older person, but they do happen to the vast majority of them. In fact, one study of older adults aged 60-90 found that 95% of them showed signs of these changes on brain MRI.
In other words, if your older parent ever gets an MRI of the head, he or she will probably show some signs of these changes.
So this is a condition that older adults and families should know about. Furthermore, these changes have been associated with problems of consequence to older adults, including:
- Cognitive decline,
- Problems with walking or balance,
- Strokes,
- Vascular dementia.
Now, perhaps the best technical term for what I’m referring to is “cerebral small vessel disease.” But many other synonyms are used by the medical community — especially in radiology reports. They include:
- White matter disease
- Small vessel ischemic disease
- Brain lesions
- Periventricular white matter changes
- Perivascular chronic ischemic white matter disease of aging
- Chronic microvascular changes, chronic microvascular ischemic changes
- Chronic microvascular ischemia
- White matter hyperintensities
- Age-related white matter changes
- Leukoaraiosis
In this post, I will explain what all older adults and their families should know about this extremely common condition related to the brain health of older adults.
In particular, I’ll address the following frequently asked questions:
- What is cerebral small vessel disease (SVD)?
- What are the symptoms of cerebral SVD?
- How is cerebral small vessel disease related to vascular dementia and cerebrovascular accidents?
- What causes cerebral SVD?
- How can cerebral SVD be treated or prevented?
- Should you request an MRI if you’re concerned about cerebral SVD?
I will also address what you can do, if you are concerned about cerebral SVD for yourself or an older loved one.
What is cerebral small vessel disease?
Cerebral small vessel disease (SVD) is an umbrella term covering a variety of abnormalities related to small blood vessels in the brain. Because most brain tissue appears white on MRIs, these abnormalities were historically referred to as “white matter changes” or “white matter disease.”
Per this medical review article, specific examples of cerebral SVD include “lacunar infarcts” (which are a type of small stroke), “white matter hyperintensities” (which are a radiological finding), and “cerebral microbleeds” (which means bleeding in the brain from a very small blood vessel).
In many cases, cerebral SVD seems to be a consequence of atherosclerosis affecting the smaller blood vessels that nourish brain tissue. Just as one’s larger blood vessels in the heart or elsewhere can accumulate plaque, inflammation, and chronic damage over the years, so can the smaller blood vessels.
Such chronic damage can lead the small blood vessels in the brain to become blocked (which starves brain cells of oxygen, and which we technically call ischemia), or to leak (which causes bleeding, which we call hemorrhage and can damage nearby brain cells).
When little bits of brain get damaged in these ways, they can change appearance on radiological scans. So when an MRI report says “white matter disease,” this means the radiologist is seeing signs that probably indicate cerebral SVD.
(Note: In this podcast episode, a UCSF brain health expert explains that although cerebral small vessel disease is probably the most common cause of white matter changes in older adults, it’s not the only condition that can cause such changes. )
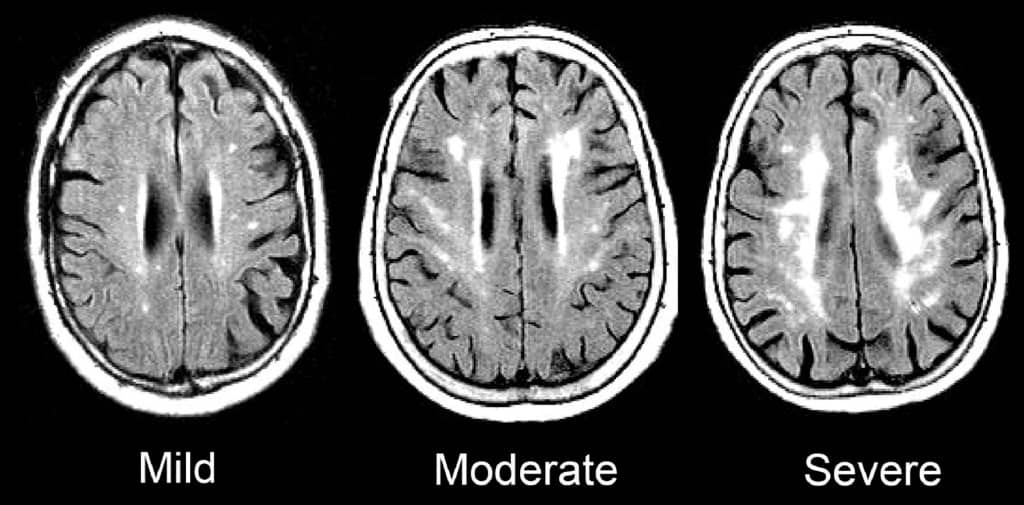
Such signs of SVD may be described as “mild”, “moderate,” or “severe/extensive,” depending on how widespread they are.
Here is an enlargement of a good image, from the BMJ article “Changes in white matter as determinant of global functional decline in older independent outpatients.”
What are the symptoms of cerebral small vessel disease?
The severity of symptoms tends to correspond to whether radiological imaging shows the white matter changes to be mild, moderate, or severe.
Many older adults with cerebral SVD will have no noticeable symptoms. This is sometimes called “silent” SVD.
But many problems have been associated with cerebral SVD, especially when it is moderate or severe. These include:
- Cognitive impairment. Several studies, such as this one, have found that cerebral SVD is correlated with worse scores on the Mini-Mental State Exam. When problems with thinking skills are associated with SVD, this can be called “vascular cognitive impairment.”
- Problems with walking and balance. White matter lesions have been repeatedly associated with gait disturbances and mobility difficulties. A 2013 study found that moderate or severe cerebral SVD was associated with a decline in gait and balance function.
- Strokes. A 2010 meta-analysis concluded that white matter hyperintensities are associated with a more than two-fold increase in the risk of stroke.
- Depression. White matter changes have been associated with a higher risk of depression in older people, and may represent a contributor to depression that is particular to having first-time depression in later life.
- Vascular dementia. Signs of cerebral SVD are associated with both having vascular dementia, and eventually developing vascular dementia.
- Other dementias. Research suggests that cerebral SVD is also associated with an increased risk — or increased severity — of other forms of dementia, such as Alzheimer’s disease. Autopsy studies have confirmed that many older adults with dementia show signs of both Alzheimer’s pathology and cerebral small vessel disease.
- Transition to disability or death. In a 2009 study of 639 non-disabled older persons (mean age 74), over a three-year follow-up period, 29.5% of participants with severe white matter changes and 15.1% of participants with moderate white matter changes developed disabilities or died. In comparison, only 10.5% of participants with mild white matter changes transitioned to disability or death over three years. The researchers concluded that severity of cerebral SVD is an important risk factor for overall decline in older adults.
So what does this all mean, in terms of symptoms and cerebral SVD? Here’s how I would boil it down:
1.Overall, older adults with any of the problems listed above have a high probability of having cerebral SVD.
2. But, many older adults with cerebral SVD on MRI are asymptomatic, and do not notice any difficulties. This is especially true of aging adults with mild cerebral SVD.
3. Older adults with cerebral SVD are at increased risk of developing the problems above, often within a few years time. This is especially true of people with moderate or severe cerebral SVD.
How is cerebral small vessel disease related to vascular dementia and cerebrovascular accidents?
The term “vascular dementia” means having dementia that is mostly due to having had problems with the blood vessels in the brain.
(For more on the definition of dementia and vascular dementia, see here: Beyond Alzheimer’s: Common Types of Dementia in Aging.)
The brain has some large blood vessels; when a person develops a clot or bleed related to a large blood vessel, this causes a major stroke, also known as a cerebrovascular accident.
It is possible to get dementia after a major stroke. However, in older adults, it’s probably more common to develop vascular dementia due to injuries to the small vessels of the brain. But again, as I explained above: not everyone with signs of cerebral small vessel disease ends up developing cognitive impairment or dementia.
What causes cerebral small vessel disease?
This is a topic of intense research, and the experts in this area tend to really nerd out when discussing it. (Read the scholarly papers listed below to see what I mean.) One reason it’s difficult to give an exact answer is that cerebral SVD is a broad umbrella term that encompasses many different types of problems with the brain’s small blood vessels.
Still, certain risk factors for developing cerebral SVD have been identified. Many overlap with risk factors for stroke. They include:
- Hypertension
- Dyslipidemia (e.g. high cholesterol)
- Atrial fibrillation
- Cerebral amyloid angiopathy
- Diabetes
- Smoking
- Age
- Inflammation
There is also evidence that Alzheimer’s disease and cerebral small vessel disease frequently co-exist in older adults, and might interact to accelerate cognitive decline.
How can cerebral small vessel disease be treated or prevented?
Experts are still trying to figure out the answers to this question, and research into the prevention of cerebral SVD is ongoing.
Since worsening of white matter disease is often associated with clinical problems, experts are also trying to determine how we might prevent, or delay, the progression of SVD in older adults.
Generally, experts recommend that clinicians consider treating any underlying risk factors. In most cases, this means detecting and treating any traditional risk factors for stroke.
(For more on identifying and addressing stroke risk factors, see How to Address Cardiovascular Risk Factors for Better Brain Health: 12 Risks to Know & 5 Things to Do.)
To date, studies of hypertension treatment to prevent the progression of white matter changes have shown mixed results. It appears that treating high blood pressure can slow the progression of brain changes in some people. But such treatment may be less effective in people who are older than 80, or who already have severe cerebral SVD.
In other words, your best bet for preventing or slowing down cerebral SVD may be to properly treat high blood pressure and other risk factors before you are 80, or otherwise have significant SVD.
Furthermore, experts don’t yet agree on how low to go, when it comes to optimal blood pressure for an older person with cerebral small vessel disease. (This article explains why this has been difficult to determine.)
For now, to prevent the occurrence or progression of cerebral small vessel disease, it’s reasonable to start by observing the hypertension guidelines considered reasonable for most older adults: treat to a target of systolic blood pressure less than 150mm/Hg.
Whether to treat high blood pressure — and other cardiovascular risk factors — more aggressively should depend on an older person’s particular health circumstances. I explain a step-by-step process you can use (with links to related research) here: 6 Steps to Better High Blood Pressure Treatment for Older Adults.
You can also learn more about the research on CSVD and the effect of treating blood pressure here: The relation between antihypertensive treatment and progression of cerebral small vessel disease.
Not necessarily. In my opinion, older adults should only get MRIs of the brain if the following two things are true:
- They are experiencing worrisome clinical symptoms, and
- The results of the MRI are needed to decide on how to treat the person.
For most older adults, an MRI showing signs of cerebral SVD will not, in of itself, change the management of medical problems.
If you have high blood pressure, you should consider treatment. If you are having difficulties with walking or balance, signs of cerebral SVD do not rule out the possibility of other common causes of walking problems, such as medication side-effects, foot pain, neuropathy, and so forth.
What if you’re concerned about memory or thinking problems? Well, you probably will find signs of cerebral SVD on an MRI, just because this is a common finding in all older adults, and it’s especially common in people who are experiencing cognitive changes.
However, the MRI cannot tell you whether the cognitive changes you are noticing are only due to cerebral SVD, versus due to developing Alzheimer’s disease, versus due one of the many other dementia mimics. You will still need to pursue a careful evaluation for cognitive impairment. And no matter what the MRI shows, you will likely need to consider optimizing cardiovascular risk factors.
So in most cases, a brain MRI just to check for cerebral SVD is probably not a good idea.
However, if an MRI is indicated for other reasons, you may find out that an older person has mild, moderate, or severe signs of cerebral SVD. In this case, especially if the cerebral SVD is moderate or severe, you’ll want to consider taking steps to reduce stroke risk, and also to monitor for cognitive changes and increased disability.
What to do if you’re worried about cerebral small vessel disease
If you are worried about cerebral SVD, for yourself or for an older relative, here a few things you can do:
- Talk to your doctor about your concerns. You may want to discuss your options for optimizing vascular risk factors, including high blood pressure, high cholesterol, high blood sugar, smoking, and others. For more on identifying and addressing stroke risk factors, see How to Address Cardiovascular Risk Factors for Better Brain Health: 12 Risks to Know & 5 Things to Do.
- Remember that exercise, a healthy diet (such as the Mediterranean diet), good sleep, stress reduction, and many other non-pharmacological approaches can help manage vascular risk factors. Lifestyle approaches are safe and usually benefit your health in lots of ways. Medications to treat high blood pressure and cholesterol should be used judiciously.
- If an MRI of the brain is clinically indicated — or if one has recently been done — ask the doctor to help you understand how the findings may correspond to any worrisome symptoms you’ve noticed. But if you’ve been worried about cognitive impairment or falls, remember that such problems are usually multi-factorial (i.e. they have multiple causes). So it’s best to make sure the doctors have checked for all other common contributors to thinking problems and/or falls.
If you want to learn still more about cerebral small vessel disease, here are some scholarly articles on the subject:
- CNS small vessel disease: A clinical review (2019)
- Mechanisms underlying sporadic cerebral small vessel disease: insights from neuroimaging
- Causes and consequences of cerebral small vessel disease. The RUN DMC study
- Vascular Contributions to Cognitive Impairment and Dementia: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association (2011)
- Early Cerebral Small Vessel Disease and Brain Volume, Cognition, and Gait
- Cardiovascular risk factors and small vessel disease of the brain: Blood pressure, white matter lesions, and functional decline in older persons
I also recommend listening to this very informative podcast interview, with Dr. Fanny Elahi of the UCSF Memory and Aging Center: 084 – Interview: Understanding White Matter Changes in the Aging Brain.
Note: We’ve hit 300+ comments on this article! So we’re closing comments for this article. Thank you for your interest!
Note: This article has generated a lot of questions from people under age 60. If that describes you, please read below:
- Please read the article on “Early Cerebral Small Vessel Disease,” the full article is available for free. This describes SVD found in people aged 40-75. In this study, 2-3% of participants in their 40s showed signs of cerebral SVD.
- You can check for more recent research on this topic by entering the above article at scholar.google.com, and then click the “Cited by” link to find newer articles that reference this article.
- I do not know much about cerebral SVD in younger adults; this is not the population that I personally treat nor read much about. (I’m already quite busy trying to keep up with research related to older adults.)
- As best I can tell, most of what we currently know about health outcomes related to cerebral SVD is based on the studies of older adults. It is not clear to me whether people with cerebral SVD at younger ages should expect similar outcomes. I will not be able to answer most questions related to cerebral SVD in people under age 60.
- If you are concerned about what caused your MRI findings, or what they might mean for the future, please don’t ask me to tell you, because I don’t have these kinds of answers and I cannot quickly find them online.
- You should start by talking to your usual doctors, and perhaps a neurologist.
- If you would like to learn more, consider finding someone specialized in white matter disease in younger adults (e.g. someone doing and publishing research on this topic). Such experts are usually based at an academic medical center. Good luck!



Leslie Riddle says
Can living at high altitude (9500 ft past 4 years-sea level prior to that) cause or contribute to chronic microvascular ischemia of the brain? Pt is 57 yr old female with hx of 3 concussions w/loss of consciousness for several minutes, new dx Crohn’s disease after several yrs IBS, surgical menopause, fibromyalgia, CRPS, mononucleosis July 2017 (to ER thinking might be a stroke). Night time hypoxia requiring O2 for sleep.
TIA!
Leslie Kernisan, MD MPH says
Hm, I’m not really sure what the effect of living at high altitude might be. This summary from the American College of Cardiology says “Albeit with limited evidence is, high altitude exposure seems to pose a risk of cerebral ischemia for patients who already have suffered an ischemic stroke; both because of the direct effect of hypoxia, and due to a reduced cerebrovascular reactivity.”
Otherwise: concussions, inflammation, these are all things that could aggravate or damage small blood vessels in the brain. This situation sounds likely to be “multifactorial.” Good luck!
Luba says
Hello Dr. Kernisan,
I just received MRI with contrast report which says there is no suspicious intraparenchymal, leptomeningldeal, or dural based enhancement. Than it says: this is suspected to reflect the sequela of chronic microangiopathic disease. I am 53 years old female in fairly good health (have Hashimoto disease, and horrible headache/ migraine for the last few months), low blood pressure, normal cholesterol, etc., what is my prognosis and what should I do? I appreciate your advise very much. Thank you for your time.
Leslie Kernisan, MD MPH says
Sorry for your headaches and recent health concerns. Unfortunately, it’s not possible for me to tell you your prognosis or what you should do. “Chronic microangiopathic disease” does basically mean cerebral small vessel disease, but you will still need to work with your doctors to find out what is likely to be the cause. Prognosis and what to do really depends on what is the cause of the problem.
You may also want to ask if your headaches and/or Hashimoto’s might be related to the signs of small vessel damage. Good luck!
Gregg says
Hello Dr Kernisan
My primary doctor ordered am MRI of my brain not sure why but I suppose it’s related to dementia being prevelant in my family as my father had dementia and recently snuck out of the house only to be killed in a car accident later that day on a train track. My report says severe confluent periventricular / subcortial white matter T2 hyperintensity. It also says moderate cerebellar atrophy with ex vacuo dialation of the fourt ventricle. Can’t get an appointment for 2 weeks as my Dr is out of town. Any clarification on these findings would be helpful until I see my primary in a couple of weeks.
Leslie Kernisan, MD MPH says
Sorry to hear of your father’s death.
Unfortunately, I’m not able to clarify the findings, to interpret them one would have to know more about your medical history and symptoms, and also best to have more training in neurology than I do.
I would definitely recommend asking a lot of questions once you do get a chance to see your doctor or another specialist. Be sure they explain what might be going on with your brain, what their plan is for further evaluation (if any), and what they recommend, to help you maintain your brain as best you can.
Good luck!
Jean Newberry says
Good morning,
I have a question for you. This is the result from my husband (62 years old) MRI report done Oct. of last year.
( There is mild enlargement ventricular system and subarachnoid spaces with mild to moderate periventricular and subcortical white matter gliosis. There is no restricted diffusion or mass effect. The craniocervical junction is normal. The flow voids of the major
intracranial vascular structures are grossly normal. Extracranial soft tissues are normal.
Impression: Mild atrophy and chronic small vessel ischemic changes without evidence of an acute abnormality.)
His PCP informed him that it is normal, no mini strokes, while the neurologist states he has had several mini strokes. We are of course going with what the neuro says. But why would we get two different opinions? He is having a lot of balance and falling issues. He is diabetic (severely), no high blood pressure, does have high cholesterol. Thank you for your time.
Leslie Kernisan, MD MPH says
Hm, I can’t say for sure why the two doctors are telling you something different. It’s possible that they have a different idea in mind of what is a “mini-stroke.” The PCP may think of that term as referring to transient ischemic attacks, rather than as referring to radiological signs of cerebral small vessel disease. The PCP may also be conflating “normal” with “common,” as your husband’s radiology report doesn’t sound very unusual.
You may want to ask the PCP about this issue, just to give him/her a chance to clarify things and maintain good communication and trust with you.
Sorry for the confusion and good luck!
Rick Rivera says
Dr.Kernisan,
I am a 71 year old man that has diabetes Type2 and take Crestor for high cholesterol
, Invokamet for diabetes & Mybetriq for incontinence…im a pretty independent person and do exercise watch my weight and im starting to get ischemic vein disease.. With the right side of my (head) brain experiencing pain..
Is there medication for this and should i get an MRI to make sure that its not something else?
Leslie Kernisan, MD MPH says
Sorry but it’s not possible for me to answer your questions. If you are having a new pain in your head or elsewhere, you need to start by seeing your health provider or another clinician, for a more in-depth interview and physical exam. Lots of different things can cause pain. Then the clinician should be able to advise you regarding which medication might help, and can formulate an opinion as to whether there is an indication for getting an MRI.
Good luck!
James says
Large issues with gait and balance, urinary issues and 2 incidences of Optic neuritis
MRI ordered due to ‘probable’ multiple sclerosis, however no demyelination noticed. Vascular issues mentioned, Neuro app months away. GP read MRI report, ordered bloods etc slightly raised cholesterol (borderline)
He mentioned SVD and recommended statins
Any advice as I am a little confused as I am only 44?
Leslie Kernisan, MD MPH says
Sorry, but I’m not a neurologist and don’t routinely care for people of your age or with your type of medical problems. I’m sorry that you’ve been having these problems, must be difficult to have such symptoms yet no clear explanation available yet.
A neurology consultation certainly sounds like the right approach.
Your GP should be able to discuss the likely benefits and risks of statins for your situation. Generally they are well-tolerated. good luck!
Jerald Skoff says
I am 75 WI and my brother is 65 OH. We both wake up in the morning with a headache that starts in the back of the neck and sometimes radiates to the the temples. My brothers are much more severe than mine and can be non functioning pain for him. He has tried a lot of different medications with little relief.
Recently we both had MRI’s for possible tumors or other conditions. Mine did come back as fairly normal for my age (per my doctor) with:
1 Moderate SV chronic ischemic disease
2. Focus magnetic susceptibility left cerebellar hemisphere, sequelae are of remote hemorrhage.
3. No evidence for acute ischemia/infarct, mass effect, or abnormal enhancement.
My physician discussed and told me the results are normal for a 75 year old male. Yet I continue to get the headaches every morning as I awake. Mine usually get better as the day progresses. My doctor says they are stress related. I have tried different pillows (feather and “My Pillow”) to see if these help. I am a type A person so I respected his conclusion until:
My brother’s MRI was abnormal and a subsequent MRA showed a brain stem vessel that was twisted or crooked near and around his brain stem. He has since been referred to another neurologist for further evaluation. The doctor thinks that stress and/or High BP puts pressure on the stem and gives him the headache.
Is this some condition that could be hereditary? Should I have further testing (MRA) to see if I have the same condition? My headaches seem to be getting much worse and more frequent. I did have one lately that lasted through the day for 6 days straight. This prompted the MRI.
My brother’s are constant. My doctor has me now on Losartan and Adalopine for my B/P since my B/P was considered higher than normal 135/98. Now it runs in the 130/80’s range. His goal is 120/80. But still have these headaches. Have tried massage therapy and chiropractor with little relief.
Would dismiss the brain as a cause until I heard about my brother’s condition and the simularities of our symptoms. Would like to have your thoughts since your blog is the best I found on SVD. Plus, of course, I would like to know why we both get these headaches when we awake in the morning. Thank you in advance for your input. I see my doctor again on Monday Mar 5th.
Leslie Kernisan, MD MPH says
Sorry if you will not be reading my response until after your doctor’s visit; I generally am able to reply to comments twice a week.
I’m glad you have this page a good source of information about cerebral SVD. That said, I’m a geriatrician, not a neurologist, and your question really goes beyond garden-variety cerebral SVD, since you are bringing up two problems:
– persisting morning headaches
– whether you’re likely to have similar abnormalities in your posterior brain circulation (that’s the part near the brainstem) as your brother and whether this is likely to be a cause of your symptoms.
There are specialists in headaches (generally neurologists) and there are specialists in stroke and neurovascular issues (also neurologists). Either type would be far better suited to address your concerns than I — an internist and geriatrician — can be.
My guess is that consulting with a headache specialist is more likely to be productive. There are a number of different issues that could be causing your morning headaches. Just by taking a quick look in my clinical references, I see that sleep apnea can be associated with headache.
It is also possible to get headaches related to irritation of the cervical nerves that innervate the scalp. (These are sometimes called cervicogenic headaches.) Such irritation can sometimes be caused by arthritis in cervical part of the spine.
There are undoubtedly other potential causes to consider for your headaches. A properly trained clinician with experience in headaches should be able to evaluate you for “alarm symptoms” and make recommendations as to what additional evaluation you should pursue.
Otherwise, your SVD does sound common for your age. Given the remote hemorrhage in your cerebellum, it would be reasonable to pay attention to your risk factors for stroke and cardiovascular disease, as you are probably already doing.
Good luck!
Martin Dewar says
I am curious about my situation. I have been diagnosed with benign essential tremors after having checks for Parkinson’s. I have suffered from mild to moderate tremors for a while. Was sent for scans at the hospital which I was told showed nothing. I suffer from dizzy spells as well. My curiosity is because I got a hold of my diagnostic list from the doctors and on the form it states
“DatSCAN imaging ruled out any evidence of dopamine degeneration. Ruled out evidence of stroke. Some minor changes in the posterior horn of the lateral ventricle, representint small volume small vessel microangiopathy – atherosclerotic disease.”
Is this the same as cerebral small vessel disease? Just as a note I am 55 years old.
Leslie Kernisan, MD MPH says
Yes, this is the same as cerebral small vessel disease. You can ask your healthcare providers to clarify whether it appears to be mild or more significant.
As I note in the some of the comments above, some people do show signs of this when they are in their 40s or 50s.
Linda says
I am 69 years old. I do not have diabetes, high blood pressure, am not overweight and have never smoked. My cholesterol is higher than normal. I had breast cancer treatment 7years ago, including chemotherapy and hormone inhibitors. After 2 years, I still had brain fog, headache, and balance problems. A MRI showed svd t no recommendations or treatment. Now, after 7 years, I am still having same symptoms. Another MRI did not show significant difference in past 5 years. Since svd was not shown on MRI done prior to chemo, I wondered if chemo could be a factor? Neurologist could only recommend diet and exercise since I do not have common risk factors. Thank you.
Leslie Kernisan, MD MPH says
Sorry to hear of your symptoms. Chemotherapy drugs are powerful and so I suppose it’s possible that they could trigger or contribute to some small vessel disease.
I would encourage you to keep asking your clinicians to help you evaluate and manage your symptoms. If they aren’t being very helpful, consider looking for a clinician who takes more a holistic or “whole person” approach.
There may be also some treatments that are worth trying if they aren’t sure what exactly is causing your symptom. For instance, special exercises to improve balance work for a variety of older adults with balance difficulties. Similarly, there are special therapy programs that often help people experience less pain. Good luck!
Kate says
Age 75 with having hemorratic stroke at age 57. Did well with physical therphy. Five years ago had diszzness, trouble with balance and was hospitalized. Told I had Microvasular ishemic disease after MRi. I have diabieies but blood pressure is under control as is my blood sugar most of the time. Recently have been having some dizziness again, fatigue and more depression. have not had Brain MRI for 5 years. Could my DVT be getting worse or is it only age related. Starting over with new Physician as long time Physician has recently retired. I enjoy your blog so informative .
Leslie Kernisan, MD MPH says
Sorry to hear of your recent symptoms. I assume you are asking if your SVD could be getting worse (a DVT usually refers to a deep vein thrombosis).
I would say that yes, it’s quite possible that your SVD has progressed, and that could be contributing to your symptoms.
That said, there are LOTS of other causes for such symptoms in people aged 75, so I would highly recommend that you ask your new physician to carefully evaluate you for your dizziness, fatigue, and mood.
If you get another MRI, it may well show more SVD, but that still doesn’t tell you if you have another problem — e.g. with thyroid, with medication side-effects, with vitamin B12 deficiency, with electrolyte imbalances, with anemia, I could go on and on — that is causing or worsening your symptoms.
Good luck with your new physician, I hope you get a careful evaluation and some helpful guidance.