
This article is about the most common aging brain problem that you may have never heard of.
While leading a fall prevention workshop a few years ago, I mentioned that an older person’s walking and balance problems might well be related to the presence of “small vessel ischemic changes” in the brain, which are very common in aging adults. (This is also called “white matter disease.”)
This led to an immediate flurry of follow-up questions. What exactly are these changes, people wanted to know. Do they happen to every older adult? Is this the same as vascular dementia? And how they can best help their parents with cognitive decline?
Well, these types of brain lesions don’t happen to every older person, but they do happen to the vast majority of them. In fact, one study of older adults aged 60-90 found that 95% of them showed signs of these changes on brain MRI.
In other words, if your older parent ever gets an MRI of the head, he or she will probably show some signs of these changes.
So this is a condition that older adults and families should know about. Furthermore, these changes have been associated with problems of consequence to older adults, including:
- Cognitive decline,
- Problems with walking or balance,
- Strokes,
- Vascular dementia.
Now, perhaps the best technical term for what I’m referring to is “cerebral small vessel disease.” But many other synonyms are used by the medical community — especially in radiology reports. They include:
- White matter disease
- Small vessel ischemic disease
- Brain lesions
- Periventricular white matter changes
- Perivascular chronic ischemic white matter disease of aging
- Chronic microvascular changes, chronic microvascular ischemic changes
- Chronic microvascular ischemia
- White matter hyperintensities
- Age-related white matter changes
- Leukoaraiosis
In this post, I will explain what all older adults and their families should know about this extremely common condition related to the brain health of older adults.
In particular, I’ll address the following frequently asked questions:
- What is cerebral small vessel disease (SVD)?
- What are the symptoms of cerebral SVD?
- How is cerebral small vessel disease related to vascular dementia and cerebrovascular accidents?
- What causes cerebral SVD?
- How can cerebral SVD be treated or prevented?
- Should you request an MRI if you’re concerned about cerebral SVD?
I will also address what you can do, if you are concerned about cerebral SVD for yourself or an older loved one.
What is cerebral small vessel disease?
Cerebral small vessel disease (SVD) is an umbrella term covering a variety of abnormalities related to small blood vessels in the brain. Because most brain tissue appears white on MRIs, these abnormalities were historically referred to as “white matter changes” or “white matter disease.”
Per this medical review article, specific examples of cerebral SVD include “lacunar infarcts” (which are a type of small stroke), “white matter hyperintensities” (which are a radiological finding), and “cerebral microbleeds” (which means bleeding in the brain from a very small blood vessel).
In many cases, cerebral SVD seems to be a consequence of atherosclerosis affecting the smaller blood vessels that nourish brain tissue. Just as one’s larger blood vessels in the heart or elsewhere can accumulate plaque, inflammation, and chronic damage over the years, so can the smaller blood vessels.
Such chronic damage can lead the small blood vessels in the brain to become blocked (which starves brain cells of oxygen, and which we technically call ischemia), or to leak (which causes bleeding, which we call hemorrhage and can damage nearby brain cells).
When little bits of brain get damaged in these ways, they can change appearance on radiological scans. So when an MRI report says “white matter disease,” this means the radiologist is seeing signs that probably indicate cerebral SVD.
(Note: In this podcast episode, a UCSF brain health expert explains that although cerebral small vessel disease is probably the most common cause of white matter changes in older adults, it’s not the only condition that can cause such changes. )
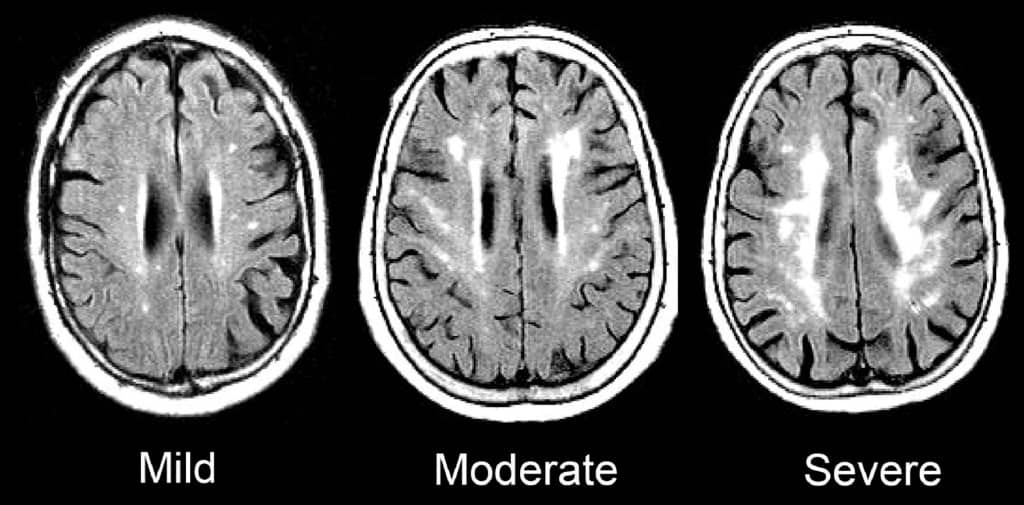
Such signs of SVD may be described as “mild”, “moderate,” or “severe/extensive,” depending on how widespread they are.
Here is an enlargement of a good image, from the BMJ article “Changes in white matter as determinant of global functional decline in older independent outpatients.”
What are the symptoms of cerebral small vessel disease?
The severity of symptoms tends to correspond to whether radiological imaging shows the white matter changes to be mild, moderate, or severe.
Many older adults with cerebral SVD will have no noticeable symptoms. This is sometimes called “silent” SVD.
But many problems have been associated with cerebral SVD, especially when it is moderate or severe. These include:
- Cognitive impairment. Several studies, such as this one, have found that cerebral SVD is correlated with worse scores on the Mini-Mental State Exam. When problems with thinking skills are associated with SVD, this can be called “vascular cognitive impairment.”
- Problems with walking and balance. White matter lesions have been repeatedly associated with gait disturbances and mobility difficulties. A 2013 study found that moderate or severe cerebral SVD was associated with a decline in gait and balance function.
- Strokes. A 2010 meta-analysis concluded that white matter hyperintensities are associated with a more than two-fold increase in the risk of stroke.
- Depression. White matter changes have been associated with a higher risk of depression in older people, and may represent a contributor to depression that is particular to having first-time depression in later life.
- Vascular dementia. Signs of cerebral SVD are associated with both having vascular dementia, and eventually developing vascular dementia.
- Other dementias. Research suggests that cerebral SVD is also associated with an increased risk — or increased severity — of other forms of dementia, such as Alzheimer’s disease. Autopsy studies have confirmed that many older adults with dementia show signs of both Alzheimer’s pathology and cerebral small vessel disease.
- Transition to disability or death. In a 2009 study of 639 non-disabled older persons (mean age 74), over a three-year follow-up period, 29.5% of participants with severe white matter changes and 15.1% of participants with moderate white matter changes developed disabilities or died. In comparison, only 10.5% of participants with mild white matter changes transitioned to disability or death over three years. The researchers concluded that severity of cerebral SVD is an important risk factor for overall decline in older adults.
So what does this all mean, in terms of symptoms and cerebral SVD? Here’s how I would boil it down:
1.Overall, older adults with any of the problems listed above have a high probability of having cerebral SVD.
2. But, many older adults with cerebral SVD on MRI are asymptomatic, and do not notice any difficulties. This is especially true of aging adults with mild cerebral SVD.
3. Older adults with cerebral SVD are at increased risk of developing the problems above, often within a few years time. This is especially true of people with moderate or severe cerebral SVD.
How is cerebral small vessel disease related to vascular dementia and cerebrovascular accidents?
The term “vascular dementia” means having dementia that is mostly due to having had problems with the blood vessels in the brain.
(For more on the definition of dementia and vascular dementia, see here: Beyond Alzheimer’s: Common Types of Dementia in Aging.)
The brain has some large blood vessels; when a person develops a clot or bleed related to a large blood vessel, this causes a major stroke, also known as a cerebrovascular accident.
It is possible to get dementia after a major stroke. However, in older adults, it’s probably more common to develop vascular dementia due to injuries to the small vessels of the brain. But again, as I explained above: not everyone with signs of cerebral small vessel disease ends up developing cognitive impairment or dementia.
What causes cerebral small vessel disease?
This is a topic of intense research, and the experts in this area tend to really nerd out when discussing it. (Read the scholarly papers listed below to see what I mean.) One reason it’s difficult to give an exact answer is that cerebral SVD is a broad umbrella term that encompasses many different types of problems with the brain’s small blood vessels.
Still, certain risk factors for developing cerebral SVD have been identified. Many overlap with risk factors for stroke. They include:
- Hypertension
- Dyslipidemia (e.g. high cholesterol)
- Atrial fibrillation
- Cerebral amyloid angiopathy
- Diabetes
- Smoking
- Age
- Inflammation
There is also evidence that Alzheimer’s disease and cerebral small vessel disease frequently co-exist in older adults, and might interact to accelerate cognitive decline.
How can cerebral small vessel disease be treated or prevented?
Experts are still trying to figure out the answers to this question, and research into the prevention of cerebral SVD is ongoing.
Since worsening of white matter disease is often associated with clinical problems, experts are also trying to determine how we might prevent, or delay, the progression of SVD in older adults.
Generally, experts recommend that clinicians consider treating any underlying risk factors. In most cases, this means detecting and treating any traditional risk factors for stroke.
(For more on identifying and addressing stroke risk factors, see How to Address Cardiovascular Risk Factors for Better Brain Health: 12 Risks to Know & 5 Things to Do.)
To date, studies of hypertension treatment to prevent the progression of white matter changes have shown mixed results. It appears that treating high blood pressure can slow the progression of brain changes in some people. But such treatment may be less effective in people who are older than 80, or who already have severe cerebral SVD.
In other words, your best bet for preventing or slowing down cerebral SVD may be to properly treat high blood pressure and other risk factors before you are 80, or otherwise have significant SVD.
Furthermore, experts don’t yet agree on how low to go, when it comes to optimal blood pressure for an older person with cerebral small vessel disease. (This article explains why this has been difficult to determine.)
For now, to prevent the occurrence or progression of cerebral small vessel disease, it’s reasonable to start by observing the hypertension guidelines considered reasonable for most older adults: treat to a target of systolic blood pressure less than 150mm/Hg.
Whether to treat high blood pressure — and other cardiovascular risk factors — more aggressively should depend on an older person’s particular health circumstances. I explain a step-by-step process you can use (with links to related research) here: 6 Steps to Better High Blood Pressure Treatment for Older Adults.
You can also learn more about the research on CSVD and the effect of treating blood pressure here: The relation between antihypertensive treatment and progression of cerebral small vessel disease.
Not necessarily. In my opinion, older adults should only get MRIs of the brain if the following two things are true:
- They are experiencing worrisome clinical symptoms, and
- The results of the MRI are needed to decide on how to treat the person.
For most older adults, an MRI showing signs of cerebral SVD will not, in of itself, change the management of medical problems.
If you have high blood pressure, you should consider treatment. If you are having difficulties with walking or balance, signs of cerebral SVD do not rule out the possibility of other common causes of walking problems, such as medication side-effects, foot pain, neuropathy, and so forth.
What if you’re concerned about memory or thinking problems? Well, you probably will find signs of cerebral SVD on an MRI, just because this is a common finding in all older adults, and it’s especially common in people who are experiencing cognitive changes.
However, the MRI cannot tell you whether the cognitive changes you are noticing are only due to cerebral SVD, versus due to developing Alzheimer’s disease, versus due one of the many other dementia mimics. You will still need to pursue a careful evaluation for cognitive impairment. And no matter what the MRI shows, you will likely need to consider optimizing cardiovascular risk factors.
So in most cases, a brain MRI just to check for cerebral SVD is probably not a good idea.
However, if an MRI is indicated for other reasons, you may find out that an older person has mild, moderate, or severe signs of cerebral SVD. In this case, especially if the cerebral SVD is moderate or severe, you’ll want to consider taking steps to reduce stroke risk, and also to monitor for cognitive changes and increased disability.
What to do if you’re worried about cerebral small vessel disease
If you are worried about cerebral SVD, for yourself or for an older relative, here a few things you can do:
- Talk to your doctor about your concerns. You may want to discuss your options for optimizing vascular risk factors, including high blood pressure, high cholesterol, high blood sugar, smoking, and others. For more on identifying and addressing stroke risk factors, see How to Address Cardiovascular Risk Factors for Better Brain Health: 12 Risks to Know & 5 Things to Do.
- Remember that exercise, a healthy diet (such as the Mediterranean diet), good sleep, stress reduction, and many other non-pharmacological approaches can help manage vascular risk factors. Lifestyle approaches are safe and usually benefit your health in lots of ways. Medications to treat high blood pressure and cholesterol should be used judiciously.
- If an MRI of the brain is clinically indicated — or if one has recently been done — ask the doctor to help you understand how the findings may correspond to any worrisome symptoms you’ve noticed. But if you’ve been worried about cognitive impairment or falls, remember that such problems are usually multi-factorial (i.e. they have multiple causes). So it’s best to make sure the doctors have checked for all other common contributors to thinking problems and/or falls.
If you want to learn still more about cerebral small vessel disease, here are some scholarly articles on the subject:
- CNS small vessel disease: A clinical review (2019)
- Mechanisms underlying sporadic cerebral small vessel disease: insights from neuroimaging
- Causes and consequences of cerebral small vessel disease. The RUN DMC study
- Vascular Contributions to Cognitive Impairment and Dementia: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association (2011)
- Early Cerebral Small Vessel Disease and Brain Volume, Cognition, and Gait
- Cardiovascular risk factors and small vessel disease of the brain: Blood pressure, white matter lesions, and functional decline in older persons
I also recommend listening to this very informative podcast interview, with Dr. Fanny Elahi of the UCSF Memory and Aging Center: 084 – Interview: Understanding White Matter Changes in the Aging Brain.
Note: We’ve hit 300+ comments on this article! So we’re closing comments for this article. Thank you for your interest!
Note: This article has generated a lot of questions from people under age 60. If that describes you, please read below:
- Please read the article on “Early Cerebral Small Vessel Disease,” the full article is available for free. This describes SVD found in people aged 40-75. In this study, 2-3% of participants in their 40s showed signs of cerebral SVD.
- You can check for more recent research on this topic by entering the above article at scholar.google.com, and then click the “Cited by” link to find newer articles that reference this article.
- I do not know much about cerebral SVD in younger adults; this is not the population that I personally treat nor read much about. (I’m already quite busy trying to keep up with research related to older adults.)
- As best I can tell, most of what we currently know about health outcomes related to cerebral SVD is based on the studies of older adults. It is not clear to me whether people with cerebral SVD at younger ages should expect similar outcomes. I will not be able to answer most questions related to cerebral SVD in people under age 60.
- If you are concerned about what caused your MRI findings, or what they might mean for the future, please don’t ask me to tell you, because I don’t have these kinds of answers and I cannot quickly find them online.
- You should start by talking to your usual doctors, and perhaps a neurologist.
- If you would like to learn more, consider finding someone specialized in white matter disease in younger adults (e.g. someone doing and publishing research on this topic). Such experts are usually based at an academic medical center. Good luck!



Bob Summers says
I am 77 years old Caus. male ,recently went to see a Doctor about Peripheral Neuropathy. In May 2017 MRI revealed right brain diffuse atrophy with Periventricular deep white matter changes. Past Medical history includes “Arthritis, Depression, Gout, Hypertension, Multiple gastric Ulcers, severe Chronic disability for PTSD, EKG (March 2018) reported right bundle branch block with inferior T-wave changes, and multiple level of neuroforaminal stenosis” In November 2018 (Recent) on examination “Alert, and undergoing significant social Stressors., MMSE 23/30, Higher cognitive functions are good, fund of Knowledge appropriate, Language intact, Obese and well developed, normal cephalic and atraumatic, cooperative, no apparent distress.” Taking Statins and Blood pressure medications. VISIT Diagnoses: Late onset Alzheimer’s disease without behavioral disturbance, Polyneuropathy, Intention tremors, Vitamin D deficiency, Abnormal EKG. Is this likely not AD, but related to PTSD and while matter disease. If so, what further action would you advise.
Leslie Kernisan, MD MPH says
Well, I explain how we diagnose dementia in the article here: How We Diagnose Dementia: The Practical Basics to Know.
From what you wrote, it’s not clear to me that all the right steps were taken, so you may want to ask the doctor some extra questions about how he or she reached his/her diagnostic conclusion. Good luck!
Bob Summers says
Thank you. I have a consult for a second opinion. For my assistance, what steps appear to you to be missing in this first medical review? I plan on taking your advise and asking for some clarification on how the “diagnostic conclusion” was reached, especially with the second opinion. Again, thank you.
Leslie Kernisan, MD MPH says
The article on dementia diagnosis explains the five criteria that must be met to diagnose dementia. I would recommend asking your health providers to clarify how they assessed each and reached their conclusion.
I also have an article on 10 causes of cognitive impairment that might be helpful:
Cognitive Impairment in Aging: 10 Common Causes & 10 Things the Doctor Should Check
Lastly, I would recommend you get a trusted family member or friend to accompany you, to take notes and help you ask the right questions. Good luck!
Tanweer says
Loved ur article sir . My father crashed in doctor’s clinic . After1 minute he regained consciousness but felt weak n dis-oriented for few hrs . Nw he is doing fine .. also he hd high fever during that time .. doctor said he had a convulsion ..
we were scared suspecting TIA or ministroke we ordered MRi which says periventricular n subcortical hyperdensities ..
Ur comments sir
Leslie Kernisan, MD MPH says
“Periventricular and subcortical hyperdensities” would be consistent with “white matter changes” and the other terms for MRI findings consistent with cerebral small vessel disease.
What the MRI cannot tell you is if a TIA was the cause of his syncope. There are many reasons that an older person can lose consciousness, so he needs a careful evaluation. Good luck!
Jason says
My dad has vascular dementia is 72 years old (diagnosed 68) he never had any of the risk factors: blood pressure, being overweight, diet, drinking, smoked lightly many years ago and lack of exercise.
He still got it.
Cochrane says statins don’t prevent dementia or cognitive decline.
Instead of cholestorol being the cause isn’t it more likely leaky blood vessels caused by endothelial dysfunction and failure of the pericytes cells?
Leslie Kernisan, MD MPH says
Sorry to hear of your father’s vascular dementia. Most health problems in older adults are multi-factorial, meaning there usually isn’t a single cause and instead, there are multiple causes and contributors.
Endothelial dysfunction and problems with pericytes are part of atherosclerosis. High cholesterol can contribute to this, but there are other causes as well. See the article on cardiovascular risk factors for more.
Carolyn Goutos says
my husband(age 73) as been having some short term memory loss. he has had a MRI and the finding is that they found mild white matter and basis of chronic microvascular ischemic disease
Leslie Kernisan, MD MPH says
Yes, these MRI findings are very common in people like your husband. As I explain in the article, he should have further evaluation for his memory loss. I explain what should be checked here: Cognitive Impairment in Aging: 10 Common Causes & 10 Things the Doctor Should Check.
Fawad Saeed Shah says
Hi Dr. Kernisan. Hope you are fine and in good health. My father age is 68 and following is his MRI HEAD / BRAIN report. Please advice. Thanks.
MRI HEAD / BRAIN WITHOUT CONTRAST
Findings:
Age appropriate involutional changes are noted within the brain parenchyma.
Evidence of multifocal punctate T2 weighted/FLAIR hyperintense signals within the subcortical and
periventricular white matter suggestive of white matter ischemic changes secondary to small vessel
disease.
No evidence of acute infarction, intracranial bleed or mass effect.
No hydrocephalous, midline shift or cerebral edema.
Thalami and basal ganglia are showing normal signals.
Cerebellum and brain stem are returning normal signals.
Major vascular flow voids and basal cisterns are preserved.
Vestibulo-cochlear nerve complexes appear unremarkable bilaterally.
Retention cyst is noted within the left maxillary antrum.
Mucosal thickening is identified involving the left maxillary and bilateral ethmoid sinuses.
Rest of the visualized paranasal sinuses and mastoid air cells are clear.
Impression:
No evidence of acute infarction, intracranial bleed or mass effect.
Evidence of white matter ischemic changes secondary to small vessel disease
Leslie Kernisan, MD MPH says
The MRI findings sound consistent with cerebral small vessel disease. I cannot tell you what this means or what to do; that all depends on his other health conditions, his symptoms, why the test was ordered in the first place, and more. It is the responsibility of the ordering physician and/or his usual health provider to explain the findings to your family and make suggestions. If you are concerned about it progressing, ask what they recommend to reduce the risk. If you are wondering whether this explains some symptom or problem you’ve noticed, ask them that. Good luck.
Fawad Saeed Shah says
Thank you very much for the reply.
Last year in July 2017 he was unconscious 2 times. Doctors found that this is because of heart and he needs pacemaker. We also want to make sure that everything is OK with brain that’s why we did MRI. Then pacemaker was implanted last year Sep 2017.
But still after pacemaker father is feeling headache and heaviness in brain.
We shown MRI report to doctors but same reply that report is OK. One doctor said that is due to chemical imbalance in brain. One doctor said that is due to depression but father said he is happy in his life and no depression.
Then this year Feb (8 months before) he had by pass surgery. His Coronary artery was blocked 95%.
Still his brain problem is same feeling headache and heaviness. When he start walking he is feeling like he will fell down but after some time he is feeling fine and continue his walking.
Thanks.
Monica Cattapan says
Hello, I am deeply concerned about my future and was hoping you could provide me with some answers.
I am a woman aged 44 years old and recently had an MRI on my brain and ears because of the following symptoms:
Dizziness
Loss of balance
Hearing difficulties
Severe short term memory loss
Headaches
I have no history of high blood pressure, do not smoke, do not consume alcohol nor ever had a cholesterol problem. My father however, did suffer from Alzheimer’s and died aged 82, following diagnosis 3 years earlier.
The report from my MRI results state that:
There are multiple foci of T2 hyperintensity are present in the deep white matter of both cerebral hemispheres. Prominent perivascular space or choroid fissure cyst in right temporal region.
Can you please provide me with information and what does this mean? my regular doctor told me I have nothing to worry about.
Thank you, l look forward to hearing from you.
Monica Cattapan says
I’m sorry I forgot to mention that the final conclusion of the MRI report states “multifocal areas of T2 signal increase consistent with small vessel disease”
Leslie Kernisan, MD MPH says
Sorry but I really do not have any clinical experience with abnormal MRI findings in people your age.
I do think that for something that either worries you a lot or seems unusual for your age group, it can be a good idea to get a second opinion. You might want to consult with a neurologist, perhaps at an academic medical center. UCSF and some of the other well-established academic centers also offer remote second opinions. Good luck!
Monica Cattapan says
Thank you for your response.
Kindest regards
Monica Cattapan
chris says
hypoplastic left vertebral artery with mri showing focal gliosis at right parieto ocipetal region with adjoining dilated cortical sulci-likely sequelae to hypoxia related changes with additional symptoms of vertigo and vomiting and sudden profound sensorineural hearing loss in left ear and moderate hearing loss in right ear . what this condition shows is it stroke, tia or something else
Leslie Kernisan, MD MPH says
Sorry but I’m not a neurologist or a neuroradiologist. Vomiting and “sudden profound sensorineural hearing loss” does not sound typical of the type of common cerebral small vessel disease that I describe in this article. I would recommend you consult in-person with a neurologist.
Patricia Young says
Hello, My dad will be 81 & just had an MRI r/t cognitive deficits, gait instability. He also has low b12 levels. Would this combination cause the SVD? Below is his MRI result. I read it to say he has had ministrokes. Thank you
Mild prominence of the ventricular sulcal system commensurate with underlying volume loss is noted. There is remote lacunar type infarctions noted within the cerebellar hemispheres bilaterally as well as within the right basal ganglia. There is punctate areas of periventricular subcortical signal abnormality. While nonspecific, this is typically attributed to small vessel ischemic change. Remainder of the brain parenchyma is normal in signal. Suprasellar and basilar cisterns are patent. Within limitations of an
unenhanced study, there is no findings to suggest parenchymal mass or mass effect. Orbits and globes are unremarkable.
IMPRESSION:
1. No acute intracranial abnormality identified
2. Mild to moderate volume loss with superimposed small vessel ischemic changes.
Leslie Kernisan, MD MPH says
Sorry to hear of your father’s difficulties. As I explain in the article, cerebral SVD is associated with problems such as cognitive dysfunction and gait problems, but these problems are also often caused by other issues not easily seen on MRI. In most older adults, both cognitive problems and gait problems are multifactorial. They also usually require multi-faceted interventions, to try to improve these problems.
In short, it’s possible his cerebral SVD is causing the problems you are seeing, AND he needs comprehensive evaluation to check for other causes and contributor.
So, I would recommend detailed evaluation for his cognitive problems, and also for his gait problems. If his B12 is low, then it would also usually be appropriate to treat that. Good luck!
Wayne says
I am a 61 yo healthy man recently diagnosed with Meniere’s disease. I had an MRI to r/o an acoustic neuroma, which was negative. The radiologist’s report said the MRI was normal except a “trace of mastoid effusion.” When I brought the MRI to my Neurotologist for a follow-up he was not at all concerned with the effusion but saw “a small amount of periventricular white matter disease.” He said this is normal for someone my age and was surprised the radiologist did not report this. I have no history of HPB or heart disease. I had borderline high cholesterol years ago and have had those numbers in the normal range for more than 20 years. I do not have noticeable symptoms of any cognitive decline. The Neurotologist sent a letter to my PCP summarizing our visit and noting the periventricular disease quoted above. I am somewhat concerned about the implications of the findings, but also concerned that this it is now in my permanent medical record: as I am right in the middle of applying for life and long term care insurance. Do you have any suggestions about either of these concerns? Thank you in advance!
Wayne
Leslie Kernisan, MD MPH says
Well, in terms of the findings of a “small amount of periventricular white matter disease,” that does sound very common for someone your age. If you are concerned, I would recommend reviewing your cardiovascular risk factors in general, including the lifestyle factors that are sometimes overlooked in routine clinical care. Your health providers should be able to help you determine what might need more attention from you, to minimize your risk of the cerebral SVD progressing.
I have no idea what insurance companies make of such findings, especially since the radiologist did not comment on it and technically the radiologist is more qualified to interpret the MRI than the neurologist is.
Good luck!
Geoff says
Hello Dr. Kernisan, Your article on SVD is very explanatory thank you. I’m 65 and had an MRI of my brain to confirm that there were no tumours or anything unusual going on inside my head for tinnitus (which I have). All was clear but the report said supratentorial white matter disease is excessive for age. All my blood pressure, cholesterol, diabetes etc is very good and I’m very fit and active for my age. Wanting to do what I could to improve my SVD situation I researched and now I’m taking – Coconut oil (high quality optimized for ketones), turmeric (fresh from the plant), Lions Mane Mushroom, Ginkgo Biloba (high quality), organic Pomegranate powder, Green tea and eat Broccoli whenever possible. All these products were actually recommended for alzheimer’s as i couldn’t find anything that would improve WMD. Please tell me if I’m on the right track or where I could be going wrong. I look forward to your reply.
Leslie Kernisan, MD MPH says
So, I know there seems to be a relationship between vascular brain changes and Alzheimer’s pathology in the brain, so it’s possible that using a nutritional approach recommended for Alzheimer’s might help with the cerebral small vessel disease.
I am not an expert in nutrition or supplements, I can’t speak to how likely it is that those nutritional approaches would make a difference for Alzheimer’s pathology or for cerebral small vessel disease.
You may want to consult with a clinician who does extensively research nutritional approaches. You can also search PubMed and Google Scholar to learn more about nutritional approaches for vascular disease. There is probably more published about cardiovascular disease, but there is a lot of overlap between the health of the heart’s blood vessels and the brain’s blood vessels.
You could also ask your health providers whether inflammation appears to be an issue for you (there are inflammatory markers in the blood that can be checked for). If you do show signs of inflammation in your blood, you could look into dietary approaches that reduce inflammation.
I have other suggestions in the related article on addressing cardiovascular risk factors, which addresses sleep, stress and other issues. Good luck!