
This article is about the most common aging brain problem that you may have never heard of.
While leading a fall prevention workshop a few years ago, I mentioned that an older person’s walking and balance problems might well be related to the presence of “small vessel ischemic changes” in the brain, which are very common in aging adults. (This is also called “white matter disease.”)
This led to an immediate flurry of follow-up questions. What exactly are these changes, people wanted to know. Do they happen to every older adult? Is this the same as vascular dementia? And how they can best help their parents with cognitive decline?
Well, these types of brain lesions don’t happen to every older person, but they do happen to the vast majority of them. In fact, one study of older adults aged 60-90 found that 95% of them showed signs of these changes on brain MRI.
In other words, if your older parent ever gets an MRI of the head, he or she will probably show some signs of these changes.
So this is a condition that older adults and families should know about. Furthermore, these changes have been associated with problems of consequence to older adults, including:
- Cognitive decline,
- Problems with walking or balance,
- Strokes,
- Vascular dementia.
Now, perhaps the best technical term for what I’m referring to is “cerebral small vessel disease.” But many other synonyms are used by the medical community — especially in radiology reports. They include:
- White matter disease
- Small vessel ischemic disease
- Brain lesions
- Periventricular white matter changes
- Perivascular chronic ischemic white matter disease of aging
- Chronic microvascular changes, chronic microvascular ischemic changes
- Chronic microvascular ischemia
- White matter hyperintensities
- Age-related white matter changes
- Leukoaraiosis
In this post, I will explain what all older adults and their families should know about this extremely common condition related to the brain health of older adults.
In particular, I’ll address the following frequently asked questions:
- What is cerebral small vessel disease (SVD)?
- What are the symptoms of cerebral SVD?
- How is cerebral small vessel disease related to vascular dementia and cerebrovascular accidents?
- What causes cerebral SVD?
- How can cerebral SVD be treated or prevented?
- Should you request an MRI if you’re concerned about cerebral SVD?
I will also address what you can do, if you are concerned about cerebral SVD for yourself or an older loved one.
What is cerebral small vessel disease?
Cerebral small vessel disease (SVD) is an umbrella term covering a variety of abnormalities related to small blood vessels in the brain. Because most brain tissue appears white on MRIs, these abnormalities were historically referred to as “white matter changes” or “white matter disease.”
Per this medical review article, specific examples of cerebral SVD include “lacunar infarcts” (which are a type of small stroke), “white matter hyperintensities” (which are a radiological finding), and “cerebral microbleeds” (which means bleeding in the brain from a very small blood vessel).
In many cases, cerebral SVD seems to be a consequence of atherosclerosis affecting the smaller blood vessels that nourish brain tissue. Just as one’s larger blood vessels in the heart or elsewhere can accumulate plaque, inflammation, and chronic damage over the years, so can the smaller blood vessels.
Such chronic damage can lead the small blood vessels in the brain to become blocked (which starves brain cells of oxygen, and which we technically call ischemia), or to leak (which causes bleeding, which we call hemorrhage and can damage nearby brain cells).
When little bits of brain get damaged in these ways, they can change appearance on radiological scans. So when an MRI report says “white matter disease,” this means the radiologist is seeing signs that probably indicate cerebral SVD.
(Note: In this podcast episode, a UCSF brain health expert explains that although cerebral small vessel disease is probably the most common cause of white matter changes in older adults, it’s not the only condition that can cause such changes. )
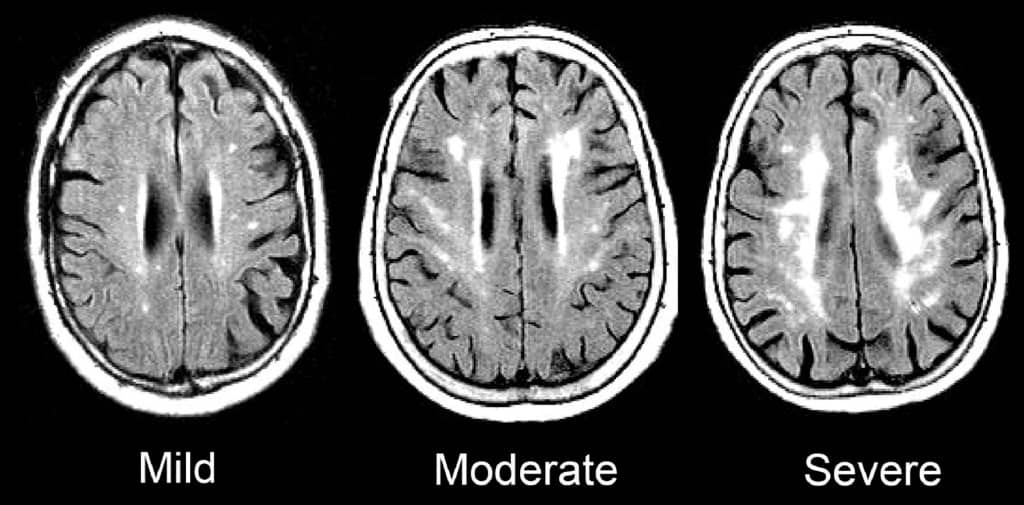
Such signs of SVD may be described as “mild”, “moderate,” or “severe/extensive,” depending on how widespread they are.
Here is an enlargement of a good image, from the BMJ article “Changes in white matter as determinant of global functional decline in older independent outpatients.”
What are the symptoms of cerebral small vessel disease?
The severity of symptoms tends to correspond to whether radiological imaging shows the white matter changes to be mild, moderate, or severe.
Many older adults with cerebral SVD will have no noticeable symptoms. This is sometimes called “silent” SVD.
But many problems have been associated with cerebral SVD, especially when it is moderate or severe. These include:
- Cognitive impairment. Several studies, such as this one, have found that cerebral SVD is correlated with worse scores on the Mini-Mental State Exam. When problems with thinking skills are associated with SVD, this can be called “vascular cognitive impairment.”
- Problems with walking and balance. White matter lesions have been repeatedly associated with gait disturbances and mobility difficulties. A 2013 study found that moderate or severe cerebral SVD was associated with a decline in gait and balance function.
- Strokes. A 2010 meta-analysis concluded that white matter hyperintensities are associated with a more than two-fold increase in the risk of stroke.
- Depression. White matter changes have been associated with a higher risk of depression in older people, and may represent a contributor to depression that is particular to having first-time depression in later life.
- Vascular dementia. Signs of cerebral SVD are associated with both having vascular dementia, and eventually developing vascular dementia.
- Other dementias. Research suggests that cerebral SVD is also associated with an increased risk — or increased severity — of other forms of dementia, such as Alzheimer’s disease. Autopsy studies have confirmed that many older adults with dementia show signs of both Alzheimer’s pathology and cerebral small vessel disease.
- Transition to disability or death. In a 2009 study of 639 non-disabled older persons (mean age 74), over a three-year follow-up period, 29.5% of participants with severe white matter changes and 15.1% of participants with moderate white matter changes developed disabilities or died. In comparison, only 10.5% of participants with mild white matter changes transitioned to disability or death over three years. The researchers concluded that severity of cerebral SVD is an important risk factor for overall decline in older adults.
So what does this all mean, in terms of symptoms and cerebral SVD? Here’s how I would boil it down:
1.Overall, older adults with any of the problems listed above have a high probability of having cerebral SVD.
2. But, many older adults with cerebral SVD on MRI are asymptomatic, and do not notice any difficulties. This is especially true of aging adults with mild cerebral SVD.
3. Older adults with cerebral SVD are at increased risk of developing the problems above, often within a few years time. This is especially true of people with moderate or severe cerebral SVD.
How is cerebral small vessel disease related to vascular dementia and cerebrovascular accidents?
The term “vascular dementia” means having dementia that is mostly due to having had problems with the blood vessels in the brain.
(For more on the definition of dementia and vascular dementia, see here: Beyond Alzheimer’s: Common Types of Dementia in Aging.)
The brain has some large blood vessels; when a person develops a clot or bleed related to a large blood vessel, this causes a major stroke, also known as a cerebrovascular accident.
It is possible to get dementia after a major stroke. However, in older adults, it’s probably more common to develop vascular dementia due to injuries to the small vessels of the brain. But again, as I explained above: not everyone with signs of cerebral small vessel disease ends up developing cognitive impairment or dementia.
What causes cerebral small vessel disease?
This is a topic of intense research, and the experts in this area tend to really nerd out when discussing it. (Read the scholarly papers listed below to see what I mean.) One reason it’s difficult to give an exact answer is that cerebral SVD is a broad umbrella term that encompasses many different types of problems with the brain’s small blood vessels.
Still, certain risk factors for developing cerebral SVD have been identified. Many overlap with risk factors for stroke. They include:
- Hypertension
- Dyslipidemia (e.g. high cholesterol)
- Atrial fibrillation
- Cerebral amyloid angiopathy
- Diabetes
- Smoking
- Age
- Inflammation
There is also evidence that Alzheimer’s disease and cerebral small vessel disease frequently co-exist in older adults, and might interact to accelerate cognitive decline.
How can cerebral small vessel disease be treated or prevented?
Experts are still trying to figure out the answers to this question, and research into the prevention of cerebral SVD is ongoing.
Since worsening of white matter disease is often associated with clinical problems, experts are also trying to determine how we might prevent, or delay, the progression of SVD in older adults.
Generally, experts recommend that clinicians consider treating any underlying risk factors. In most cases, this means detecting and treating any traditional risk factors for stroke.
(For more on identifying and addressing stroke risk factors, see How to Address Cardiovascular Risk Factors for Better Brain Health: 12 Risks to Know & 5 Things to Do.)
To date, studies of hypertension treatment to prevent the progression of white matter changes have shown mixed results. It appears that treating high blood pressure can slow the progression of brain changes in some people. But such treatment may be less effective in people who are older than 80, or who already have severe cerebral SVD.
In other words, your best bet for preventing or slowing down cerebral SVD may be to properly treat high blood pressure and other risk factors before you are 80, or otherwise have significant SVD.
Furthermore, experts don’t yet agree on how low to go, when it comes to optimal blood pressure for an older person with cerebral small vessel disease. (This article explains why this has been difficult to determine.)
For now, to prevent the occurrence or progression of cerebral small vessel disease, it’s reasonable to start by observing the hypertension guidelines considered reasonable for most older adults: treat to a target of systolic blood pressure less than 150mm/Hg.
Whether to treat high blood pressure — and other cardiovascular risk factors — more aggressively should depend on an older person’s particular health circumstances. I explain a step-by-step process you can use (with links to related research) here: 6 Steps to Better High Blood Pressure Treatment for Older Adults.
You can also learn more about the research on CSVD and the effect of treating blood pressure here: The relation between antihypertensive treatment and progression of cerebral small vessel disease.
Not necessarily. In my opinion, older adults should only get MRIs of the brain if the following two things are true:
- They are experiencing worrisome clinical symptoms, and
- The results of the MRI are needed to decide on how to treat the person.
For most older adults, an MRI showing signs of cerebral SVD will not, in of itself, change the management of medical problems.
If you have high blood pressure, you should consider treatment. If you are having difficulties with walking or balance, signs of cerebral SVD do not rule out the possibility of other common causes of walking problems, such as medication side-effects, foot pain, neuropathy, and so forth.
What if you’re concerned about memory or thinking problems? Well, you probably will find signs of cerebral SVD on an MRI, just because this is a common finding in all older adults, and it’s especially common in people who are experiencing cognitive changes.
However, the MRI cannot tell you whether the cognitive changes you are noticing are only due to cerebral SVD, versus due to developing Alzheimer’s disease, versus due one of the many other dementia mimics. You will still need to pursue a careful evaluation for cognitive impairment. And no matter what the MRI shows, you will likely need to consider optimizing cardiovascular risk factors.
So in most cases, a brain MRI just to check for cerebral SVD is probably not a good idea.
However, if an MRI is indicated for other reasons, you may find out that an older person has mild, moderate, or severe signs of cerebral SVD. In this case, especially if the cerebral SVD is moderate or severe, you’ll want to consider taking steps to reduce stroke risk, and also to monitor for cognitive changes and increased disability.
What to do if you’re worried about cerebral small vessel disease
If you are worried about cerebral SVD, for yourself or for an older relative, here a few things you can do:
- Talk to your doctor about your concerns. You may want to discuss your options for optimizing vascular risk factors, including high blood pressure, high cholesterol, high blood sugar, smoking, and others. For more on identifying and addressing stroke risk factors, see How to Address Cardiovascular Risk Factors for Better Brain Health: 12 Risks to Know & 5 Things to Do.
- Remember that exercise, a healthy diet (such as the Mediterranean diet), good sleep, stress reduction, and many other non-pharmacological approaches can help manage vascular risk factors. Lifestyle approaches are safe and usually benefit your health in lots of ways. Medications to treat high blood pressure and cholesterol should be used judiciously.
- If an MRI of the brain is clinically indicated — or if one has recently been done — ask the doctor to help you understand how the findings may correspond to any worrisome symptoms you’ve noticed. But if you’ve been worried about cognitive impairment or falls, remember that such problems are usually multi-factorial (i.e. they have multiple causes). So it’s best to make sure the doctors have checked for all other common contributors to thinking problems and/or falls.
If you want to learn still more about cerebral small vessel disease, here are some scholarly articles on the subject:
- CNS small vessel disease: A clinical review (2019)
- Mechanisms underlying sporadic cerebral small vessel disease: insights from neuroimaging
- Causes and consequences of cerebral small vessel disease. The RUN DMC study
- Vascular Contributions to Cognitive Impairment and Dementia: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association (2011)
- Early Cerebral Small Vessel Disease and Brain Volume, Cognition, and Gait
- Cardiovascular risk factors and small vessel disease of the brain: Blood pressure, white matter lesions, and functional decline in older persons
I also recommend listening to this very informative podcast interview, with Dr. Fanny Elahi of the UCSF Memory and Aging Center: 084 – Interview: Understanding White Matter Changes in the Aging Brain.
Note: We’ve hit 300+ comments on this article! So we’re closing comments for this article. Thank you for your interest!
Note: This article has generated a lot of questions from people under age 60. If that describes you, please read below:
- Please read the article on “Early Cerebral Small Vessel Disease,” the full article is available for free. This describes SVD found in people aged 40-75. In this study, 2-3% of participants in their 40s showed signs of cerebral SVD.
- You can check for more recent research on this topic by entering the above article at scholar.google.com, and then click the “Cited by” link to find newer articles that reference this article.
- I do not know much about cerebral SVD in younger adults; this is not the population that I personally treat nor read much about. (I’m already quite busy trying to keep up with research related to older adults.)
- As best I can tell, most of what we currently know about health outcomes related to cerebral SVD is based on the studies of older adults. It is not clear to me whether people with cerebral SVD at younger ages should expect similar outcomes. I will not be able to answer most questions related to cerebral SVD in people under age 60.
- If you are concerned about what caused your MRI findings, or what they might mean for the future, please don’t ask me to tell you, because I don’t have these kinds of answers and I cannot quickly find them online.
- You should start by talking to your usual doctors, and perhaps a neurologist.
- If you would like to learn more, consider finding someone specialized in white matter disease in younger adults (e.g. someone doing and publishing research on this topic). Such experts are usually based at an academic medical center. Good luck!



Shirley Johnson says
Hi, I had a small stroke three months ago, I was told I have moderate svd . My cholesterol is being dealt with but Atorvastatin has given me shocking stiffness and I have tried leaving it off for two weeks which cured the stiffness but when I return to tell my doctor I’m hoping there is an alternative because simvastatin affected me when I was put on it many years ago . I am seventy one and do thank you for all your helpful info. For ages I have a slightly unsteady feeling and awful head and eyes which I have always put down to my sensitive sinuses and pollution, so this information gives an answer to what it may be all about. My husband is convinced its all fine and I’m no different, but he does admit I have become more withdrawn
Leslie Kernisan, MD MPH says
Sorry to hear of your stroke. Statins are associated with a lower risk of repeat cardiovascular event, but they are just one of many things one can do to reduce the risk. Even though you didn’t tolerate atorvastatin or simvastatin, you may want to ask your doctor about trying one of the other statins, such as pravastatin or fluvastatin, because some research suggests these are less likely to cause side-effects. good luck!
Shirley Johnson says
Thanks, my doctor has given me a different one, not as good called ezetimibe. Maybe I could ask about the ones you mentioned when I attend my follow up at the stroke clinic.
Thank you
Shirley
Lynn A Bochart says
Two years ago, when I was 70 I talked to my family doctor about the fact that I felt like I was beginning to have some memory problems. He ordered an MRI of the brain. Findings were Moderate to severe chronic microangiopathy. My doctor just stated that this was common and nothing could be done. Do you agree with that statement? What type of doctor should I talk to about this? I would like to be pro-active to deal with this if at all possible. I don’t think I have had any changes in memory issues since I had the MRI done. Thanks.
Leslie Kernisan, MD MPH says
So first of all, if the concern is memory problems, then we would recommend a comprehensive evaluation for that specifically. An MRI is only a small part of the evaluation. I explain the evaluation here:
Cognitive Impairment in Aging: 10 Common Causes & 10 Things the Doctor Should Check
In terms of what your MRI findings mean and what should be done, this has to be correlated to your symptoms and the rest of your health history. In many cases, what is appropriate is to take steps to address cardiovascular risk, and I cover those here:
How to Address Cardiovascular Risk Factors for Better Brain Health: 12 Risks to Know & 5 Things to Do.
Good luck!
Cheryl says
Hi I am 60 and my mri report says chronic microvascular white matter changes and hyperintonsities but when I talked to my Dr she said my mri was normal. Does this sound right? Should I get a second opinion?
Leslie Kernisan, MD MPH says
Hm, hard to say. As I note in the article, these kinds of white matter changes are very common in older adults. Whether to consider it concerning really would depend on the amount of changes and whether their pattern seemed uncommon. Your health providers should also consider whether you are having any worrisome symptoms, and the rest of your health history. You could consider asking your doctor whether these results mean you should consider changing some aspect of your lifestyle or health care plan. If you are concerned, you could also consider a second opinion. Good luck!
Sam says
Hi Leslie,
Happy new year. My dad, age 65, engineer and love to work, started to lose his balance for walking on 21 December 2018. The Drs said it is mid ear nerve issue which is viral or flu and gave him some medication like Betahistine. we did MRI for him. The report as follow:
MR study of brain using axial T1, T2 and sagittal T2 and coronal T2 and axial FLAIR images:
Senile cortical brain atrophy accompanied by few small vessel ischemic foci in deep white matter.
No diffusion restriction confirming recent infraction is seen. There is no space occupying lesion. Both 7/8 nerve complexes, pituitary fossa, both orbits & optic nerves are normal in shape and signal intensity./kh/z*
I came across your article here and this small vessel ischemic foci maybe same as what you mentioned here. I appreciate your advice if you think we need to do more things for him. his thinking, talking, hearing, eyes all good without issue. only lost his balance for walking and dizzy when he standing since 21st Dec till now 11th Jan, it is not fixed at all.
I can send you the MRI pics if you like to have a look at them.
Thanks in advance,
Sam
Leslie Kernisan, MD MPH says
Sorry to hear of your father’s recent balance difficulties. I am not a neurologist or radiologist, so I don’t review MRIs and I really can’t give specific advice on what should be done. As noted in the article, these kinds of MRI changes are very common in older adults and hence it’s difficult to know whether a particular symptom is due to white matter changes or not. I would recommend continuing to work with his doctors. You may also want to consider a second opinion, especially if he’s not getting better and the symptoms are quite significant. Good luck!
Kathy wilkins says
My Husband was diagnosed with sever small vessel ischemic in 2016. He is now 70 yrs old. He is not able to have a clear conversation because of cognitive problems. He is inconvenient. He seems to understands what I’m saying to him and does recognize me the family and people he’s known. He is still very ambulatory and also very combative. Is his being combative a symptom of the disease?
Thank You
Leslie Kernisan, MD MPH says
If his cognitive problems are significant enough to interfere with daily life (sounds like they are, since he is having trouble with conversations), then that would be concerning for dementia. White matter lesions and small vessel disease in the brain can cause vascular dementia, but there are other causes of dementia too. For more on what causes cognitive problems or difficult behaviors, see these articles:
Cognitive Impairment in Aging: 10 Common Causes & 10 Things the Doctor Should Check
7 Steps to Managing Difficult Dementia Behaviors (Safely & Without Medications)
In general, I would recommend looking for a support group, for people caring with a person with cognitive impairment. This will help you cope with difficult behaviors, which are fairly common when the brain is damaged in late-life. Good luck!
Sam says
Thanks for your response.i will check with other doctors too. I am just wondering is these white matter has only one symptom ie waking and balance only or it need to have multiple symptoms like problem in talking, hearing, seeing. Thanks again
Leslie Kernisan, MD MPH says
How many symptoms might be associated with white matter changes is quite variable, among other things it would depend on the extent of the white matter changes and where they are in the brain.
Don Rustic says
Dear Dr. Kernisan,
Thank you so much for this informative article. You are doing a great service to the patient in need. The God will bless you more to serve the Mankind!
My Wife (30Yrs) was Identified of having Pituitary Micro adenoma two years back, with the support of MRI Scan.
She was prescribe for taken medicine of Cabagolin (Carberlin 0.5mg) for two years for the Nodule size around 9mm x 8mm. Then the Medicine was stopped due to Pregnancy. Now it is 4 months after her first delivery.
Our Endocrinologist advice to repeat MRI before starting the Carberlin again. Last week we did the MRI & the results were shown as below.
1. Normal MRI scan of Pituitary gland. There are no nonenhancing Lesions in the Pituitary gland to suggest Pituitary Microadenoma.
2. Sub-Cortical white matter changes most consistent with ischemic gliosis secondary to small vessel disease. Suggest medical advice.
The above two points are the impression of the report by the Radiologist. Please advise on the second point. Is it serious issue to concern? Any medical treatments to be taken? Since our family doctor not considered must on this matter.
Please Doctor advise us. God Bless You!
Leslie Kernisan, MD MPH says
Sorry to hear of your wife’s health concerns.
I really don’t know much about MRI changes in people her age. I would recommend consulting a neurologist, preferably one who is an academic medical center or otherwise has experience with more unusual cases. Good luck!
Gil says
Great article I found it helpful. I’m what you call a migraine survivalist, usually having 3 to 4 a month. This pass summer I was having severe head pain with numbness in my face that was not due to my migraine. I had a MIR done and found some area with small vessel ischemic changes. The problem I have is that I have different interpretation from two doctors. One was like, yes you have changes happening, but not to worry. The other was like I have one foot on a banana peal and the other foot in the grave. As you can see I’m at a lost. I’m 56 years old and other wise in good health. I enclose the finding of the MRI, again a great article.
IMPRESSION: No evidence of acute infarct, hemorrhage or mass effect. Periventricular white matter small vessel ischemic changes with scattered foci of abnormal signal intensity in the white matter which may represent foci of ischemia or gliosis. Less likely this may represent demyelination. Followup examination is suggested in 3-6 months.
Leslie Kernisan, MD MPH says
Glad you found the article helpful. Without knowing more about your health conditions, and also how significant are the white matter changes (are they mild, moderate, or severe), it’s hard for me to have an opinion as to how much worry sounds warranted.
I will say that in my experience, for “garden variety” white matter changes, they don’t usually recommend a follow-up examination in 3-6 months. You may want to ask your doctors more questions about this. You could also take your scan to be interpreted by a different neuroradiologist.
I would also recommend asking your doctors to clarify what they think is the cause of your white matter changes. At age 56, making changes to your cardiovascular risk factors could potentially make a difference; your health providers should be able to advise you.
Last but not least: we have a podcast episode coming out in about a month, on white matter changes, featuring one of my UCSF colleagues who specializes in studying this condition. She has a lot of good insights on what these changes might mean, and also there are some ongoing research studies looking for volunteers. You may want to tune in and listen once it’s available.
Good luck!
Dee Grant says
Dr. Kernisan, Thank you so much for this informative article. I feel so much better after having read it. Perhaps I’m just aging normally. Accepting this with grace is the hardest thing to do. I appreciate your use of layman’s terms so that as a non medical professional I could grasp an understanding of cerebral SVDs. My heart felt thanks.
Leslie Kernisan, MD MPH says
Thank you for this comment, I’m so glad you found the article helpful.
Annie says
Hi Dr. K. I want to seek for your advice. My mom is 69 years old. She has hypertension and diabetes mellitus. She is currently taking atenolol as her maintenance, while diet modification for her DM. She is having difficulty walking which started last year. It became worse this year. Her brain CT Scan showed Bilateral Periventricular White Matter Changes due to chronic small vessel disease. Cerebral and cerebellar atrophy. Not unusual for patient’s age. Atherosclerosis. I am wondering if this small vessel disease is the reason why she is having difficulty walking. We already consulted a neurologist who just said that there is nothing wrong with her scan, and that she only needs exercise. Please advice. Thank you.
Leslie Kernisan, MD MPH says
There are many reasons why someone her age with a history of high BP and diabetes would have some difficulty walking. It is also common for difficulty walking to be multifactorial, meaning there are several things causing/contributing to it.
Her chronic small vessel disease may be part of it, and even if it is, exercise is still a good idea because it improves walking and mobility in many older adults, regardless of the underlying causes for the walking problems.
There may be other treatable issues causing her walking difficulties. You could try getting a second opinion, or otherwise you could ask her current neurologist to help you understand all the possible contributors to her walking problems. You could also ask if they see anything specifically abnormal on her neurological exam, such as loss of sensation in her feet, abnormal reflexes, etc.
Good luck!
Kathy Smith says
I just had a brain MRI due to moderate and worsening diplopia. The results: “Brain: No restricted diffusion is seen to suggest acute infarction. There is no acute intracranial hemorrhage, cerebral edema, or midline shift. Age-related cerebral and cerebellar substance loss is present. Scattered increased T2 and FLAIR signal within the periventricular and subcortical white matter is
present. This is nonspecific but likely related to chronic microangiopathic ischemic change.”
Would this explain my double vision? It seems to be my only clear symptom although, at age 69, I’ve been concerned about some mild cognitive changes, as well. Periodically, I have migraine auras that rarely lead to full-blown headaches; however, I know that’s a vascular problem. I have very low blood pressure, low cholesterol, never smoked, no diabetes and am in otherwise good health.
Thanks for any feedback!
Leslie Kernisan, MD MPH says
Diplopia means double vision. I am not a neurologist but my understanding is that the problem is usually related to either the muscles directing the eyes or the nerves that control those muscles. Usually, a good exam to assess the nerve function for those little muscles controlling the eyes is needed.
Your MRI findings do not sound particularly explanatory of your double vision. I would recommend following up with your usual health provider to ask more questions. You may also want to consider seeing a neurologist, if you haven’t already done so. Good luck!
Mavis says
My husband, 68, was diagnosed with Parkinson’s Disease about 4 years ago. Recently he saw a movement disorder specialist/neurologist and was told he did not have Parkinson’s but instead had Vascular Parkinsonism caused by small infarcts deep in the brain, showing up as white matter lesions. I can find very little information on this. Is this diagnosis the same as Cerebral Small Vessel Disease, and where can I find more information? Thank you.
Leslie Kernisan, MD MPH says
Vascular parkinsonism means having Parkinson’s-like symptoms (often stiffness, slowness, gait problems, falls, and perhaps tremors) due to some type of small vessel injury affecting the parts of the brain often impaired by Parkinsons. In true Parkinson’s, the problem starts with abnormal accumulation of certain proteins in certain specific regions of the brain that control movement. (There are also other conditions that cause Parkinson’s-like symptoms.)
I would say that vascular Parkinsonism could be considered a manifestation of a type of cerebral small vessel disease affecting a certain part of the brain.
Here’s a scholarly article that might be helpful
Vascular parkinsonism: Deconstructing a syndrome
I’m not an expert on vascular Parkinsonism or what to expect, but I have occasionally had patients with this diagnosis. One downside is that the Parkinson’s symptoms do not tend to respond to Parkinson’s medications. On the other hand, the person won’t necessarily get worse and progress in the same way that Parkinson’s often progresses. Hope this helps, and good luck!