
This article is about the most common aging brain problem that you may have never heard of.
While leading a fall prevention workshop a few years ago, I mentioned that an older person’s walking and balance problems might well be related to the presence of “small vessel ischemic changes” in the brain, which are very common in aging adults. (This is also called “white matter disease.”)
This led to an immediate flurry of follow-up questions. What exactly are these changes, people wanted to know. Do they happen to every older adult? Is this the same as vascular dementia? And how they can best help their parents with cognitive decline?
Well, these types of brain lesions don’t happen to every older person, but they do happen to the vast majority of them. In fact, one study of older adults aged 60-90 found that 95% of them showed signs of these changes on brain MRI.
In other words, if your older parent ever gets an MRI of the head, he or she will probably show some signs of these changes.
So this is a condition that older adults and families should know about. Furthermore, these changes have been associated with problems of consequence to older adults, including:
- Cognitive decline,
- Problems with walking or balance,
- Strokes,
- Vascular dementia.
Now, perhaps the best technical term for what I’m referring to is “cerebral small vessel disease.” But many other synonyms are used by the medical community — especially in radiology reports. They include:
- White matter disease
- Small vessel ischemic disease
- Brain lesions
- Periventricular white matter changes
- Perivascular chronic ischemic white matter disease of aging
- Chronic microvascular changes, chronic microvascular ischemic changes
- Chronic microvascular ischemia
- White matter hyperintensities
- Age-related white matter changes
- Leukoaraiosis
In this post, I will explain what all older adults and their families should know about this extremely common condition related to the brain health of older adults.
In particular, I’ll address the following frequently asked questions:
- What is cerebral small vessel disease (SVD)?
- What are the symptoms of cerebral SVD?
- How is cerebral small vessel disease related to vascular dementia and cerebrovascular accidents?
- What causes cerebral SVD?
- How can cerebral SVD be treated or prevented?
- Should you request an MRI if you’re concerned about cerebral SVD?
I will also address what you can do, if you are concerned about cerebral SVD for yourself or an older loved one.
What is cerebral small vessel disease?
Cerebral small vessel disease (SVD) is an umbrella term covering a variety of abnormalities related to small blood vessels in the brain. Because most brain tissue appears white on MRIs, these abnormalities were historically referred to as “white matter changes” or “white matter disease.”
Per this medical review article, specific examples of cerebral SVD include “lacunar infarcts” (which are a type of small stroke), “white matter hyperintensities” (which are a radiological finding), and “cerebral microbleeds” (which means bleeding in the brain from a very small blood vessel).
In many cases, cerebral SVD seems to be a consequence of atherosclerosis affecting the smaller blood vessels that nourish brain tissue. Just as one’s larger blood vessels in the heart or elsewhere can accumulate plaque, inflammation, and chronic damage over the years, so can the smaller blood vessels.
Such chronic damage can lead the small blood vessels in the brain to become blocked (which starves brain cells of oxygen, and which we technically call ischemia), or to leak (which causes bleeding, which we call hemorrhage and can damage nearby brain cells).
When little bits of brain get damaged in these ways, they can change appearance on radiological scans. So when an MRI report says “white matter disease,” this means the radiologist is seeing signs that probably indicate cerebral SVD.
(Note: In this podcast episode, a UCSF brain health expert explains that although cerebral small vessel disease is probably the most common cause of white matter changes in older adults, it’s not the only condition that can cause such changes. )
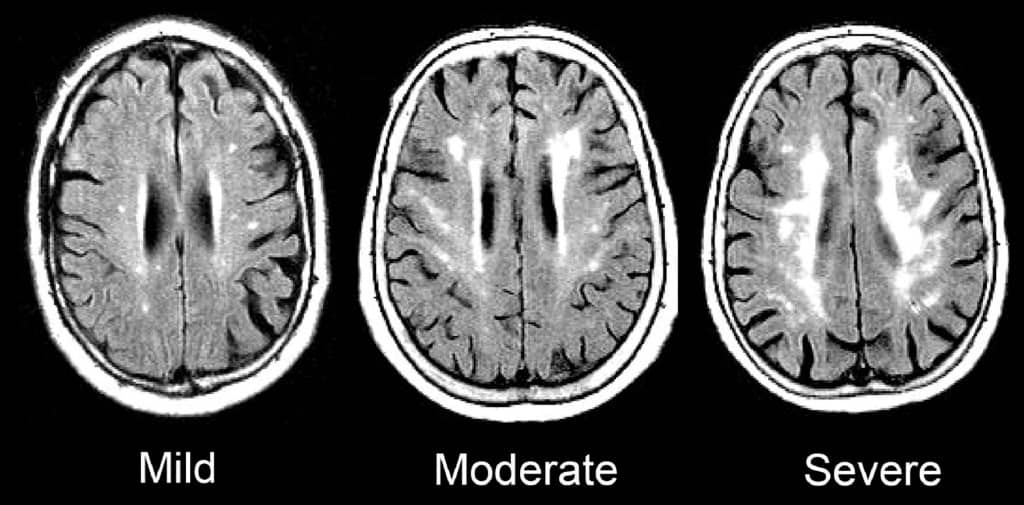
Such signs of SVD may be described as “mild”, “moderate,” or “severe/extensive,” depending on how widespread they are.
Here is an enlargement of a good image, from the BMJ article “Changes in white matter as determinant of global functional decline in older independent outpatients.”
What are the symptoms of cerebral small vessel disease?
The severity of symptoms tends to correspond to whether radiological imaging shows the white matter changes to be mild, moderate, or severe.
Many older adults with cerebral SVD will have no noticeable symptoms. This is sometimes called “silent” SVD.
But many problems have been associated with cerebral SVD, especially when it is moderate or severe. These include:
- Cognitive impairment. Several studies, such as this one, have found that cerebral SVD is correlated with worse scores on the Mini-Mental State Exam. When problems with thinking skills are associated with SVD, this can be called “vascular cognitive impairment.”
- Problems with walking and balance. White matter lesions have been repeatedly associated with gait disturbances and mobility difficulties. A 2013 study found that moderate or severe cerebral SVD was associated with a decline in gait and balance function.
- Strokes. A 2010 meta-analysis concluded that white matter hyperintensities are associated with a more than two-fold increase in the risk of stroke.
- Depression. White matter changes have been associated with a higher risk of depression in older people, and may represent a contributor to depression that is particular to having first-time depression in later life.
- Vascular dementia. Signs of cerebral SVD are associated with both having vascular dementia, and eventually developing vascular dementia.
- Other dementias. Research suggests that cerebral SVD is also associated with an increased risk — or increased severity — of other forms of dementia, such as Alzheimer’s disease. Autopsy studies have confirmed that many older adults with dementia show signs of both Alzheimer’s pathology and cerebral small vessel disease.
- Transition to disability or death. In a 2009 study of 639 non-disabled older persons (mean age 74), over a three-year follow-up period, 29.5% of participants with severe white matter changes and 15.1% of participants with moderate white matter changes developed disabilities or died. In comparison, only 10.5% of participants with mild white matter changes transitioned to disability or death over three years. The researchers concluded that severity of cerebral SVD is an important risk factor for overall decline in older adults.
So what does this all mean, in terms of symptoms and cerebral SVD? Here’s how I would boil it down:
1.Overall, older adults with any of the problems listed above have a high probability of having cerebral SVD.
2. But, many older adults with cerebral SVD on MRI are asymptomatic, and do not notice any difficulties. This is especially true of aging adults with mild cerebral SVD.
3. Older adults with cerebral SVD are at increased risk of developing the problems above, often within a few years time. This is especially true of people with moderate or severe cerebral SVD.
How is cerebral small vessel disease related to vascular dementia and cerebrovascular accidents?
The term “vascular dementia” means having dementia that is mostly due to having had problems with the blood vessels in the brain.
(For more on the definition of dementia and vascular dementia, see here: Beyond Alzheimer’s: Common Types of Dementia in Aging.)
The brain has some large blood vessels; when a person develops a clot or bleed related to a large blood vessel, this causes a major stroke, also known as a cerebrovascular accident.
It is possible to get dementia after a major stroke. However, in older adults, it’s probably more common to develop vascular dementia due to injuries to the small vessels of the brain. But again, as I explained above: not everyone with signs of cerebral small vessel disease ends up developing cognitive impairment or dementia.
What causes cerebral small vessel disease?
This is a topic of intense research, and the experts in this area tend to really nerd out when discussing it. (Read the scholarly papers listed below to see what I mean.) One reason it’s difficult to give an exact answer is that cerebral SVD is a broad umbrella term that encompasses many different types of problems with the brain’s small blood vessels.
Still, certain risk factors for developing cerebral SVD have been identified. Many overlap with risk factors for stroke. They include:
- Hypertension
- Dyslipidemia (e.g. high cholesterol)
- Atrial fibrillation
- Cerebral amyloid angiopathy
- Diabetes
- Smoking
- Age
- Inflammation
There is also evidence that Alzheimer’s disease and cerebral small vessel disease frequently co-exist in older adults, and might interact to accelerate cognitive decline.
How can cerebral small vessel disease be treated or prevented?
Experts are still trying to figure out the answers to this question, and research into the prevention of cerebral SVD is ongoing.
Since worsening of white matter disease is often associated with clinical problems, experts are also trying to determine how we might prevent, or delay, the progression of SVD in older adults.
Generally, experts recommend that clinicians consider treating any underlying risk factors. In most cases, this means detecting and treating any traditional risk factors for stroke.
(For more on identifying and addressing stroke risk factors, see How to Address Cardiovascular Risk Factors for Better Brain Health: 12 Risks to Know & 5 Things to Do.)
To date, studies of hypertension treatment to prevent the progression of white matter changes have shown mixed results. It appears that treating high blood pressure can slow the progression of brain changes in some people. But such treatment may be less effective in people who are older than 80, or who already have severe cerebral SVD.
In other words, your best bet for preventing or slowing down cerebral SVD may be to properly treat high blood pressure and other risk factors before you are 80, or otherwise have significant SVD.
Furthermore, experts don’t yet agree on how low to go, when it comes to optimal blood pressure for an older person with cerebral small vessel disease. (This article explains why this has been difficult to determine.)
For now, to prevent the occurrence or progression of cerebral small vessel disease, it’s reasonable to start by observing the hypertension guidelines considered reasonable for most older adults: treat to a target of systolic blood pressure less than 150mm/Hg.
Whether to treat high blood pressure — and other cardiovascular risk factors — more aggressively should depend on an older person’s particular health circumstances. I explain a step-by-step process you can use (with links to related research) here: 6 Steps to Better High Blood Pressure Treatment for Older Adults.
You can also learn more about the research on CSVD and the effect of treating blood pressure here: The relation between antihypertensive treatment and progression of cerebral small vessel disease.
Not necessarily. In my opinion, older adults should only get MRIs of the brain if the following two things are true:
- They are experiencing worrisome clinical symptoms, and
- The results of the MRI are needed to decide on how to treat the person.
For most older adults, an MRI showing signs of cerebral SVD will not, in of itself, change the management of medical problems.
If you have high blood pressure, you should consider treatment. If you are having difficulties with walking or balance, signs of cerebral SVD do not rule out the possibility of other common causes of walking problems, such as medication side-effects, foot pain, neuropathy, and so forth.
What if you’re concerned about memory or thinking problems? Well, you probably will find signs of cerebral SVD on an MRI, just because this is a common finding in all older adults, and it’s especially common in people who are experiencing cognitive changes.
However, the MRI cannot tell you whether the cognitive changes you are noticing are only due to cerebral SVD, versus due to developing Alzheimer’s disease, versus due one of the many other dementia mimics. You will still need to pursue a careful evaluation for cognitive impairment. And no matter what the MRI shows, you will likely need to consider optimizing cardiovascular risk factors.
So in most cases, a brain MRI just to check for cerebral SVD is probably not a good idea.
However, if an MRI is indicated for other reasons, you may find out that an older person has mild, moderate, or severe signs of cerebral SVD. In this case, especially if the cerebral SVD is moderate or severe, you’ll want to consider taking steps to reduce stroke risk, and also to monitor for cognitive changes and increased disability.
What to do if you’re worried about cerebral small vessel disease
If you are worried about cerebral SVD, for yourself or for an older relative, here a few things you can do:
- Talk to your doctor about your concerns. You may want to discuss your options for optimizing vascular risk factors, including high blood pressure, high cholesterol, high blood sugar, smoking, and others. For more on identifying and addressing stroke risk factors, see How to Address Cardiovascular Risk Factors for Better Brain Health: 12 Risks to Know & 5 Things to Do.
- Remember that exercise, a healthy diet (such as the Mediterranean diet), good sleep, stress reduction, and many other non-pharmacological approaches can help manage vascular risk factors. Lifestyle approaches are safe and usually benefit your health in lots of ways. Medications to treat high blood pressure and cholesterol should be used judiciously.
- If an MRI of the brain is clinically indicated — or if one has recently been done — ask the doctor to help you understand how the findings may correspond to any worrisome symptoms you’ve noticed. But if you’ve been worried about cognitive impairment or falls, remember that such problems are usually multi-factorial (i.e. they have multiple causes). So it’s best to make sure the doctors have checked for all other common contributors to thinking problems and/or falls.
If you want to learn still more about cerebral small vessel disease, here are some scholarly articles on the subject:
- CNS small vessel disease: A clinical review (2019)
- Mechanisms underlying sporadic cerebral small vessel disease: insights from neuroimaging
- Causes and consequences of cerebral small vessel disease. The RUN DMC study
- Vascular Contributions to Cognitive Impairment and Dementia: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association (2011)
- Early Cerebral Small Vessel Disease and Brain Volume, Cognition, and Gait
- Cardiovascular risk factors and small vessel disease of the brain: Blood pressure, white matter lesions, and functional decline in older persons
I also recommend listening to this very informative podcast interview, with Dr. Fanny Elahi of the UCSF Memory and Aging Center: 084 – Interview: Understanding White Matter Changes in the Aging Brain.
Note: We’ve hit 300+ comments on this article! So we’re closing comments for this article. Thank you for your interest!
Note: This article has generated a lot of questions from people under age 60. If that describes you, please read below:
- Please read the article on “Early Cerebral Small Vessel Disease,” the full article is available for free. This describes SVD found in people aged 40-75. In this study, 2-3% of participants in their 40s showed signs of cerebral SVD.
- You can check for more recent research on this topic by entering the above article at scholar.google.com, and then click the “Cited by” link to find newer articles that reference this article.
- I do not know much about cerebral SVD in younger adults; this is not the population that I personally treat nor read much about. (I’m already quite busy trying to keep up with research related to older adults.)
- As best I can tell, most of what we currently know about health outcomes related to cerebral SVD is based on the studies of older adults. It is not clear to me whether people with cerebral SVD at younger ages should expect similar outcomes. I will not be able to answer most questions related to cerebral SVD in people under age 60.
- If you are concerned about what caused your MRI findings, or what they might mean for the future, please don’t ask me to tell you, because I don’t have these kinds of answers and I cannot quickly find them online.
- You should start by talking to your usual doctors, and perhaps a neurologist.
- If you would like to learn more, consider finding someone specialized in white matter disease in younger adults (e.g. someone doing and publishing research on this topic). Such experts are usually based at an academic medical center. Good luck!



Eric M says
This one likely to be a little different.
I was tested by Donald Weaver at Toronto Western hospital.
In some areas i was perfect and in others like the CERAD i got 15/30 with a end result being 24/30 in the Folstien and 24/30 in the Montreal Cognitive testing.
He went on to say i got discrete problems with various aspects of my mental status but globally i was not too bad. Along with issues with memory that appear to be real.
He does not think i have neurodegenerative disorder ,MCi or Alzheimer’s.
He does suspect i have a vascular issue due to my mri showing chronic microangiopathy along with evidence suggesting congenital hypoplasia in certain arteries on the right side.
There is also some white matter lesions non distinct in nature
This is further complicated by the fact that he has hemochromatosis which may be contributing to increased blood viscosity.
I am 51 and have none of the risk factors for vascular problems such as smoking or hypertension.
Unfortunately that was me on a good day with bad days turning me into a mess where i can’t remember where iam for periods of time or how to count .
There is also the aphasia which is frustrating at the best of times and bad enough a few times that they think i am having a stroke.
Along with balance issues and feeling and control problems in both the left arm and leg.
I could handle things if they were stable but they can change from day to day, hour to hour or min to min.
Not to mention if i get to hot things get worse quickly.
I understand that its impossible to tell how the brain going to be affected and understand why blood rushing to cool my skin would cause things to get worse for the brain.
What i don’t get is why it varies so much at times and how i can go from a kind of normal person to some who’s brain is saying i am fine and the mouth actually saying bunny couch moon.
Having those really bad days certainly takes the fun out of like and more common days where it bounces all over are insanely frustrating , which the days were i am kind of normal seem like a breath of fresh air.
Why such a wide change at times?
PS: iam also sure i likely wandered all over the place for which i do apologize my focus is not what it use to be at times lol.
Leslie Kernisan, MD MPH says
Sorry to hear of your difficulties. Your case sounds a little uncommon, given your age and your symptoms. I’m glad you are getting a careful evaluation at what sounds like a specialty institution.
I can’t say why you experience these wide variations, especially since you’re younger than my own patients. In older adults, such variation is often reflective of having very little “cognitive reserve”, so when the person is taxed (by fatigue, a virus, a medication side-effect), the brain starts to quite noticeably malfunction. You may want to ask your health providers if something similar might be happening to you. Good luck!
Ahmed says
Good day Dr Leslie,
My mom is 65 yo. She has had an MRI, and the result is showing abnormally of Few T2 & Flair hyperintense foci are seen involving the peri-matter of cerebral hemispheres… Reflecting mild ischemic.
Could you please help us understanding the result? As we have had different doctors’ opinions.
Thanks
Leslie Kernisan, MD MPH says
Everything I can say in terms of explanations is in the article. These MRI results sound consistent with cerebral small vessel disease, perhaps mild since you mention “reflecting mild ischemic”. It is a common finding in people her age. I would recommend asking her usual doctors to explain how this MRI has helped them better evaluate whatever symptoms or issues caused them to order an MRI. Good luck!
Patti Kramer says
My husband, who is 58, has been diagnosed with small vascular disease. He has diabetes, severe neuropathy in his feet & his left foot has started turning out. He has a lot of balance issues. He can no longer walk across the room without holding onto something. He tried Physical therapy, but it seemed to make things worse. He is also experiencing memory issues. He will ask the same question that I answered just a few minutes before. Or forget things in general His initial MRI was done because the Dr was trying to figure out his dizziness. His primary Dr & the Dr who read the MRI, both thought he had MS. But the endocrinologist said it was Small vascular disease. We need to find something to help him. He spends most of his day in bed because of not feeling well & the balance issues. Do you have any suggestions of what to do or where we can get help figuring this all out? We are in Portland, OR
Thank you
Leslie Kernisan, MD MPH says
Sorry to hear of your husband’s difficulties. He does sound like a particularly complicated case. For people his age with memory problems, it can be worthwhile to be seen at a specialty center, such as a memory center or a specialty neurology clinic. (I would think a neurologist is better qualified to evaluate his symptoms than an endocrinologist.) Such special clinics are often available at academic medical centers.
Another option would be to consider a special “second opinion” service, in which one’s case is remotely reviewed by a team of elite specialists. UCSF offers this service: UCSF Second Opinion.
Good luck, I hope you get some answers soon.
Tammy Mowrer says
I am a 57 year old woman. I have suffered from sever depression anxiety and suididal tendencies for the last several years. About a year ago I started loosing my balance and my gait change considerably. When I started having symptoms with my very healthy heart I was put in the hospital for testing. Long story short after 6 months of hospital visits and tests (including MRI CT and PET scans) my local docs found nothing. I was sent to mayo and they found the CSVD. My question is, I have started stuttering. Has there been any cases where this is a symptom.
Leslie Kernisan, MD MPH says
Your case sounds quite complicated. I would recommend asking your clinicians at Mayo about the stuttering, and what might be causing it. In general, it sounds like you’re experiencing several symptoms and changes to your health. What is most important is for you to work closely with health providers who can carefully sort through what might be causing it. Good luck and take care!
Cindi Kirby says
Hi Leslie
My dad is far away – living in NZ and I am in SA. He has Chronic Fatigue. In bed 22 hours (at least) out of 24 hours. He recently had a brain scan. Results:
Diagnosis:
Hypersomnolence, probably due to OSA.
EDI: medspecg
Further to my letter of the 5th of July, Maurice has now had the CT scan done at North Shore Radiology. This shows some patchy small vessel disease only and a degree of parenchymal and cerebellar atrophy. No space occupying lesion has been demonstrated.
I suspect the intracranial findings reflect his generalised vascular disease. This could also have resulted in the memory disturbance that he has noted. Ongoing aggressive management of his vascular risk factors, particularly blood pressure and lipids, is important.
As you know I referred him for a sleep study but have not had a reply yet.
We are waiting for the overnight Sleep Apnea Test, which should be hopefully in about 5 weeks. He has brain fog, and is becoming weak. He was born in 1940, making him 78 next month. He has also had incidences of going shopping and leaving his wallet behind – on a few occasions. He walked out of the shops and didnt know which way to go (when he returned to NZ from a 3 month visit with me). He says he feels hazey. He had a quadruple bypass two years ago. He is on diabetes meds, had his gall bladder removed, is on high bp meds … so he isnt that well, so we are trying to get treatment for the chronic fatigue to begin with, but Im concerned that Dementia might be knocking. He feels best when he walks, but hasnt had the energy on most days to walk. He yawns all day. Can you explain to me what the Results to his CT scan really means. and any other suggestions and comments. Thanks, Cindi
Leslie Kernisan, MD MPH says
Sorry but I can’t really say much about his CT findings, his doctor’s interpretation sounds reasonable.
As I explain in the article, a head scan by itself cannot explain exactly why someone might be experiencing memory or thinking problems, or even low energy problems. For this, a more comprehensive evaluation is necessary. I cover cognitive evaluations here: Cognitive Impairment in Aging: 10 Common Causes & 10 Things the Doctor Should Check.
It is quite common for cognitive problems to be multifactorial, so some of it might be cerebral small vessel disease at the same as having sleep apnea, neurodegenerative brain changes (e.g. Alzheimer’s, Lewy-body changes) etc.
Good luck!
Amanda says
Could you please tell me if trauma as in auto accident with whiplash could cause the following findings on CT scan 3 years after initial CT scan did not show any findings? 72yr Male
And also what these results could mean.
-Prominent ventricles and sulci consistent with global cerebral volume loss.
-Hypoattenuation is noted in the periventricular and subcortical white matter, consistent with chronic small vessel ischemic disease.
– nonspecific calcifications are present on bilateral basal ganglia
Any insight into this is much appreciated.
Leslie Kernisan, MD MPH says
I don’t know if head trauma is associated with cerebral SVD but it sounds plausible. The MRI findings you describe in general sound quite common for an older adult in their 70s.
One question for you to consider, or to discuss with your doctors: how will investigating a potential connection between whiplash and cerebral SVD help with your current concerns? It’s not clear to me how pursuing this will help you better care for this 72 year old man. Good luck!
Nadia says
Hi. My mother had an MRI and one of its findings is :
Few nonspecific T2 high signal foci are seen in periventricular and subcortical white matter attributable to microvascular ischemic changes.
Does it mean that my mother has alzheimer’s? and She has diabete.
Thank you for your reply
Leslie Kernisan, MD MPH says
No, Alzheimer’s disease cannot be diagnosed just on the basis of an MRI. Alzheimer’s disease itself causes accumulation of beta-amyloid protein in the brain, and this is not visible with a regular MRI. What you describe sounds like cerebral small vessel disease, but perhaps only mild since they wrote “few foci”. Diabetes does affect the health of blood vessels, so it would not be surprising to see this finding in someone with diabetes.
If you are concerned about whether your mother might have clinical Alzheimer’s or another form of dementia, I have an article on that here: How We Diagnose Dementia: The Practical Basics to Know.
Diagnosing pre-clinical Alzheimer’s (which means Alzheimer’s changes in the brain but no obvious symptoms yet; the changes are known to start developing 10-15 years prior to obvious symptoms) requires specialized testing and is usually only done as part of a research study.
Nadia says
Thank you for your help٬ dear Leslie Kernisan
gary wood says
Hi i have just received a copy of my medical records, and on one page is (report summary) of (MRI pituitary with contrast) Technique pituitary protocol.
Findings
there is a scattered small vessel ischaemic change in the peripheral frontal lobes bilaterally. normal appearances of stalk and suprasellar system.
normal hypothalamus.
nb. Transcription not checked by radiologist.
i have suffered mood swings brain fog loosing words forgetting name etc. is this anything to do with that.
thanks Gary
Leslie Kernisan, MD MPH says
As I explain in the article, signs of small vessel disease in the brain are pretty non-specific. It requires a lot more information and context, along with a medical history and a physical exam, to determine how likely it is that someone’s symptoms correspond to a certain finding on imaging.
I would recommend asking your usual healthcare providers to help you understand whether these MRI findings are likely to explain your symptoms. If you are having cognitive concerns, you may also want to make sure you’ve had a thorough evaluation for this; I explain what should be involved here:
Cognitive Impairment in Aging: 10 Common Causes & 10 Things the Doctor Should Check. good luck!
Diane Malkiewicz says
Hello my 66yo husband had an MRI due to cognitive,, memory and balance issues which showed advanced chronic small vessel changes and mild generalized volume loss….we are seeing a number of specialists. He has normal blood pressure, Cholesterol, and no Diabetes. He had cervical surgery 3 years ago with some post anesthesia complications. My primary question is can he fly? We visit our young grandchildren twice a year. Thank you.
Leslie Kernisan, MD MPH says
As for as I know, having small vessel disease is not a contraindication to flying, but the safest approach would be to ask his usual health providers if there is any reason to be concerned about flying.
I will say that travel tends to be tiring, so if he’s having memory and balance problems, it’s possible that those might get worse during the trip, because those are problems that get worse when people are tired or stressed. Try to make sure he gets enough time to rest and recharge during the trip. good luck!
Elaine says
My neurosurgeon has said I have small vessels disease and more white matter than someone my age should have. I have a lot of difficulty with balance and gait. I had an MRI in January 2017 and will have another on August 14th, 2018. Will my balance ever improve? I have chronic severe depression and anxiety. Am I destined for vascular dementia?
PS……I am 63 and overweight. I am on abilify to supplement a depression medication and I continue to gain weight from this medication.
PPS. My mother has Parkinson’s , what are my chances of getting that as well?
Leslie Kernisan, MD MPH says
I would never say that someone with signs of cerebral small vessel disease is “destined” for vascular dementia. But it is certainly a risk factor as it indicates a certain amount of damage has already occurred.
In terms of your balance improving, I can’t say for sure but in general, many older adults are able to improve their balance by doing the right kinds of exercises to improve strength and balance. It’s also important to avoid medications that worsen balance, and to be assessed for other treatable health issues that can affect balance.
I’m not sure how your mother’s history of Parkinson’s would affect your own risk. I doubt it’s productive for you to spend a lot of time considering this…improving your lifestyle factors in general (e.g. addressing sleep, exercise, healthy nutrition, considering mindfulness, etc) is probably more likely to help you.
Otherwise, if you haven’t yet tried cognitive behavioral therapy for anxiety and other non-drug treatments for anxiety, that might be worth considering. Unfortunately, most medications for anxiety do increase fall risk, as do antipsychotics. That said, it’s also important for you to keep your psychiatric symptoms adequately controlled. Your health providers should be able to help you weigh your options and the related risks, regarding treatment with Abilify and other medications. Good luck!