
This article is about the most common aging brain problem that you may have never heard of.
While leading a fall prevention workshop a few years ago, I mentioned that an older person’s walking and balance problems might well be related to the presence of “small vessel ischemic changes” in the brain, which are very common in aging adults. (This is also called “white matter disease.”)
This led to an immediate flurry of follow-up questions. What exactly are these changes, people wanted to know. Do they happen to every older adult? Is this the same as vascular dementia? And how they can best help their parents with cognitive decline?
Well, these types of brain lesions don’t happen to every older person, but they do happen to the vast majority of them. In fact, one study of older adults aged 60-90 found that 95% of them showed signs of these changes on brain MRI.
In other words, if your older parent ever gets an MRI of the head, he or she will probably show some signs of these changes.
So this is a condition that older adults and families should know about. Furthermore, these changes have been associated with problems of consequence to older adults, including:
- Cognitive decline,
- Problems with walking or balance,
- Strokes,
- Vascular dementia.
Now, perhaps the best technical term for what I’m referring to is “cerebral small vessel disease.” But many other synonyms are used by the medical community — especially in radiology reports. They include:
- White matter disease
- Small vessel ischemic disease
- Brain lesions
- Periventricular white matter changes
- Perivascular chronic ischemic white matter disease of aging
- Chronic microvascular changes, chronic microvascular ischemic changes
- Chronic microvascular ischemia
- White matter hyperintensities
- Age-related white matter changes
- Leukoaraiosis
In this post, I will explain what all older adults and their families should know about this extremely common condition related to the brain health of older adults.
In particular, I’ll address the following frequently asked questions:
- What is cerebral small vessel disease (SVD)?
- What are the symptoms of cerebral SVD?
- How is cerebral small vessel disease related to vascular dementia and cerebrovascular accidents?
- What causes cerebral SVD?
- How can cerebral SVD be treated or prevented?
- Should you request an MRI if you’re concerned about cerebral SVD?
I will also address what you can do, if you are concerned about cerebral SVD for yourself or an older loved one.
What is cerebral small vessel disease?
Cerebral small vessel disease (SVD) is an umbrella term covering a variety of abnormalities related to small blood vessels in the brain. Because most brain tissue appears white on MRIs, these abnormalities were historically referred to as “white matter changes” or “white matter disease.”
Per this medical review article, specific examples of cerebral SVD include “lacunar infarcts” (which are a type of small stroke), “white matter hyperintensities” (which are a radiological finding), and “cerebral microbleeds” (which means bleeding in the brain from a very small blood vessel).
In many cases, cerebral SVD seems to be a consequence of atherosclerosis affecting the smaller blood vessels that nourish brain tissue. Just as one’s larger blood vessels in the heart or elsewhere can accumulate plaque, inflammation, and chronic damage over the years, so can the smaller blood vessels.
Such chronic damage can lead the small blood vessels in the brain to become blocked (which starves brain cells of oxygen, and which we technically call ischemia), or to leak (which causes bleeding, which we call hemorrhage and can damage nearby brain cells).
When little bits of brain get damaged in these ways, they can change appearance on radiological scans. So when an MRI report says “white matter disease,” this means the radiologist is seeing signs that probably indicate cerebral SVD.
(Note: In this podcast episode, a UCSF brain health expert explains that although cerebral small vessel disease is probably the most common cause of white matter changes in older adults, it’s not the only condition that can cause such changes. )
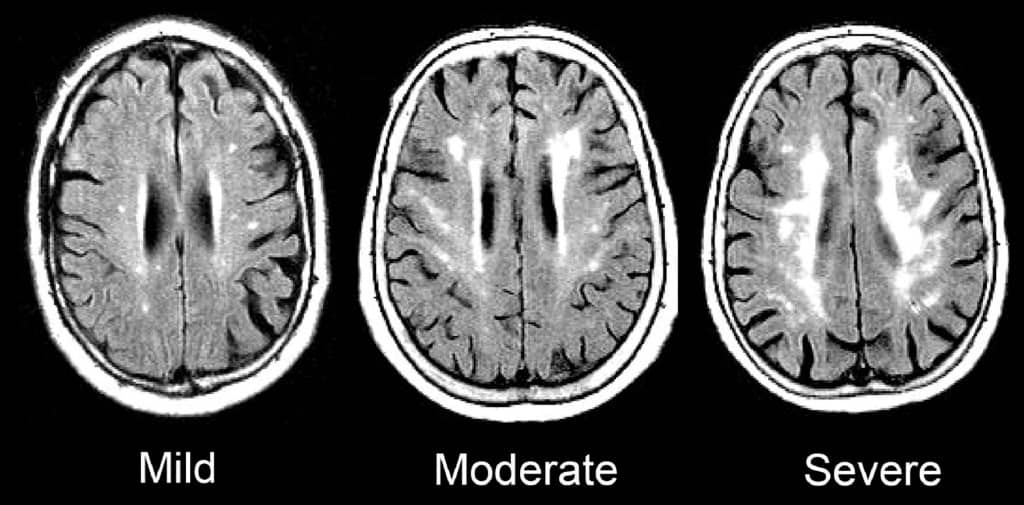
Such signs of SVD may be described as “mild”, “moderate,” or “severe/extensive,” depending on how widespread they are.
Here is an enlargement of a good image, from the BMJ article “Changes in white matter as determinant of global functional decline in older independent outpatients.”
What are the symptoms of cerebral small vessel disease?
The severity of symptoms tends to correspond to whether radiological imaging shows the white matter changes to be mild, moderate, or severe.
Many older adults with cerebral SVD will have no noticeable symptoms. This is sometimes called “silent” SVD.
But many problems have been associated with cerebral SVD, especially when it is moderate or severe. These include:
- Cognitive impairment. Several studies, such as this one, have found that cerebral SVD is correlated with worse scores on the Mini-Mental State Exam. When problems with thinking skills are associated with SVD, this can be called “vascular cognitive impairment.”
- Problems with walking and balance. White matter lesions have been repeatedly associated with gait disturbances and mobility difficulties. A 2013 study found that moderate or severe cerebral SVD was associated with a decline in gait and balance function.
- Strokes. A 2010 meta-analysis concluded that white matter hyperintensities are associated with a more than two-fold increase in the risk of stroke.
- Depression. White matter changes have been associated with a higher risk of depression in older people, and may represent a contributor to depression that is particular to having first-time depression in later life.
- Vascular dementia. Signs of cerebral SVD are associated with both having vascular dementia, and eventually developing vascular dementia.
- Other dementias. Research suggests that cerebral SVD is also associated with an increased risk — or increased severity — of other forms of dementia, such as Alzheimer’s disease. Autopsy studies have confirmed that many older adults with dementia show signs of both Alzheimer’s pathology and cerebral small vessel disease.
- Transition to disability or death. In a 2009 study of 639 non-disabled older persons (mean age 74), over a three-year follow-up period, 29.5% of participants with severe white matter changes and 15.1% of participants with moderate white matter changes developed disabilities or died. In comparison, only 10.5% of participants with mild white matter changes transitioned to disability or death over three years. The researchers concluded that severity of cerebral SVD is an important risk factor for overall decline in older adults.
So what does this all mean, in terms of symptoms and cerebral SVD? Here’s how I would boil it down:
1.Overall, older adults with any of the problems listed above have a high probability of having cerebral SVD.
2. But, many older adults with cerebral SVD on MRI are asymptomatic, and do not notice any difficulties. This is especially true of aging adults with mild cerebral SVD.
3. Older adults with cerebral SVD are at increased risk of developing the problems above, often within a few years time. This is especially true of people with moderate or severe cerebral SVD.
How is cerebral small vessel disease related to vascular dementia and cerebrovascular accidents?
The term “vascular dementia” means having dementia that is mostly due to having had problems with the blood vessels in the brain.
(For more on the definition of dementia and vascular dementia, see here: Beyond Alzheimer’s: Common Types of Dementia in Aging.)
The brain has some large blood vessels; when a person develops a clot or bleed related to a large blood vessel, this causes a major stroke, also known as a cerebrovascular accident.
It is possible to get dementia after a major stroke. However, in older adults, it’s probably more common to develop vascular dementia due to injuries to the small vessels of the brain. But again, as I explained above: not everyone with signs of cerebral small vessel disease ends up developing cognitive impairment or dementia.
What causes cerebral small vessel disease?
This is a topic of intense research, and the experts in this area tend to really nerd out when discussing it. (Read the scholarly papers listed below to see what I mean.) One reason it’s difficult to give an exact answer is that cerebral SVD is a broad umbrella term that encompasses many different types of problems with the brain’s small blood vessels.
Still, certain risk factors for developing cerebral SVD have been identified. Many overlap with risk factors for stroke. They include:
- Hypertension
- Dyslipidemia (e.g. high cholesterol)
- Atrial fibrillation
- Cerebral amyloid angiopathy
- Diabetes
- Smoking
- Age
- Inflammation
There is also evidence that Alzheimer’s disease and cerebral small vessel disease frequently co-exist in older adults, and might interact to accelerate cognitive decline.
How can cerebral small vessel disease be treated or prevented?
Experts are still trying to figure out the answers to this question, and research into the prevention of cerebral SVD is ongoing.
Since worsening of white matter disease is often associated with clinical problems, experts are also trying to determine how we might prevent, or delay, the progression of SVD in older adults.
Generally, experts recommend that clinicians consider treating any underlying risk factors. In most cases, this means detecting and treating any traditional risk factors for stroke.
(For more on identifying and addressing stroke risk factors, see How to Address Cardiovascular Risk Factors for Better Brain Health: 12 Risks to Know & 5 Things to Do.)
To date, studies of hypertension treatment to prevent the progression of white matter changes have shown mixed results. It appears that treating high blood pressure can slow the progression of brain changes in some people. But such treatment may be less effective in people who are older than 80, or who already have severe cerebral SVD.
In other words, your best bet for preventing or slowing down cerebral SVD may be to properly treat high blood pressure and other risk factors before you are 80, or otherwise have significant SVD.
Furthermore, experts don’t yet agree on how low to go, when it comes to optimal blood pressure for an older person with cerebral small vessel disease. (This article explains why this has been difficult to determine.)
For now, to prevent the occurrence or progression of cerebral small vessel disease, it’s reasonable to start by observing the hypertension guidelines considered reasonable for most older adults: treat to a target of systolic blood pressure less than 150mm/Hg.
Whether to treat high blood pressure — and other cardiovascular risk factors — more aggressively should depend on an older person’s particular health circumstances. I explain a step-by-step process you can use (with links to related research) here: 6 Steps to Better High Blood Pressure Treatment for Older Adults.
You can also learn more about the research on CSVD and the effect of treating blood pressure here: The relation between antihypertensive treatment and progression of cerebral small vessel disease.
Not necessarily. In my opinion, older adults should only get MRIs of the brain if the following two things are true:
- They are experiencing worrisome clinical symptoms, and
- The results of the MRI are needed to decide on how to treat the person.
For most older adults, an MRI showing signs of cerebral SVD will not, in of itself, change the management of medical problems.
If you have high blood pressure, you should consider treatment. If you are having difficulties with walking or balance, signs of cerebral SVD do not rule out the possibility of other common causes of walking problems, such as medication side-effects, foot pain, neuropathy, and so forth.
What if you’re concerned about memory or thinking problems? Well, you probably will find signs of cerebral SVD on an MRI, just because this is a common finding in all older adults, and it’s especially common in people who are experiencing cognitive changes.
However, the MRI cannot tell you whether the cognitive changes you are noticing are only due to cerebral SVD, versus due to developing Alzheimer’s disease, versus due one of the many other dementia mimics. You will still need to pursue a careful evaluation for cognitive impairment. And no matter what the MRI shows, you will likely need to consider optimizing cardiovascular risk factors.
So in most cases, a brain MRI just to check for cerebral SVD is probably not a good idea.
However, if an MRI is indicated for other reasons, you may find out that an older person has mild, moderate, or severe signs of cerebral SVD. In this case, especially if the cerebral SVD is moderate or severe, you’ll want to consider taking steps to reduce stroke risk, and also to monitor for cognitive changes and increased disability.
What to do if you’re worried about cerebral small vessel disease
If you are worried about cerebral SVD, for yourself or for an older relative, here a few things you can do:
- Talk to your doctor about your concerns. You may want to discuss your options for optimizing vascular risk factors, including high blood pressure, high cholesterol, high blood sugar, smoking, and others. For more on identifying and addressing stroke risk factors, see How to Address Cardiovascular Risk Factors for Better Brain Health: 12 Risks to Know & 5 Things to Do.
- Remember that exercise, a healthy diet (such as the Mediterranean diet), good sleep, stress reduction, and many other non-pharmacological approaches can help manage vascular risk factors. Lifestyle approaches are safe and usually benefit your health in lots of ways. Medications to treat high blood pressure and cholesterol should be used judiciously.
- If an MRI of the brain is clinically indicated — or if one has recently been done — ask the doctor to help you understand how the findings may correspond to any worrisome symptoms you’ve noticed. But if you’ve been worried about cognitive impairment or falls, remember that such problems are usually multi-factorial (i.e. they have multiple causes). So it’s best to make sure the doctors have checked for all other common contributors to thinking problems and/or falls.
If you want to learn still more about cerebral small vessel disease, here are some scholarly articles on the subject:
- CNS small vessel disease: A clinical review (2019)
- Mechanisms underlying sporadic cerebral small vessel disease: insights from neuroimaging
- Causes and consequences of cerebral small vessel disease. The RUN DMC study
- Vascular Contributions to Cognitive Impairment and Dementia: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association (2011)
- Early Cerebral Small Vessel Disease and Brain Volume, Cognition, and Gait
- Cardiovascular risk factors and small vessel disease of the brain: Blood pressure, white matter lesions, and functional decline in older persons
I also recommend listening to this very informative podcast interview, with Dr. Fanny Elahi of the UCSF Memory and Aging Center: 084 – Interview: Understanding White Matter Changes in the Aging Brain.
Note: We’ve hit 300+ comments on this article! So we’re closing comments for this article. Thank you for your interest!
Note: This article has generated a lot of questions from people under age 60. If that describes you, please read below:
- Please read the article on “Early Cerebral Small Vessel Disease,” the full article is available for free. This describes SVD found in people aged 40-75. In this study, 2-3% of participants in their 40s showed signs of cerebral SVD.
- You can check for more recent research on this topic by entering the above article at scholar.google.com, and then click the “Cited by” link to find newer articles that reference this article.
- I do not know much about cerebral SVD in younger adults; this is not the population that I personally treat nor read much about. (I’m already quite busy trying to keep up with research related to older adults.)
- As best I can tell, most of what we currently know about health outcomes related to cerebral SVD is based on the studies of older adults. It is not clear to me whether people with cerebral SVD at younger ages should expect similar outcomes. I will not be able to answer most questions related to cerebral SVD in people under age 60.
- If you are concerned about what caused your MRI findings, or what they might mean for the future, please don’t ask me to tell you, because I don’t have these kinds of answers and I cannot quickly find them online.
- You should start by talking to your usual doctors, and perhaps a neurologist.
- If you would like to learn more, consider finding someone specialized in white matter disease in younger adults (e.g. someone doing and publishing research on this topic). Such experts are usually based at an academic medical center. Good luck!



Michael McTeague says
My wife of 58 year old has just had an MRI scan and the report, although shows everything normal, it does state “Multiple small hyper signal intensity (SI) leions involving centrum semiovalae , corona radiata and subcortial & preventricular white matter (WM) of both frontal parietal lobes, representing deep WM ischemia due to mild small blood vessel disease” Should we be concerned or seek other medical treatment????
Leslie Kernisan, MD MPH says
You don’t say why this MRI was ordered in the first place, or whether your wife is having concerning symptoms.
If she is feeling well, I would recommend discussing the findings with her doctor and asking for help identifying and managing any risk factors for cerebral small vessel disease. Research generally suggests that treating risk factors such as high blood pressure, glucose intolerance, high cholesterol, inflammation, or lack of exercise is all more likely to have an effect when it’s done in middle-age, compared to when people are in the 80s. Good luck!
Jo wicks says
Hi there,
I’m concerned about my 66 year old mum, at the start of this year she had a bout of vertigo that lasted about 7 weeks.
Investigations included an MRI which showed narrowing of the vessels in the brain the doctors didn’t seem too concerned and said common in older people. They didn’t indicate how severe.
Eventually the vertigo cleared up.
However the vertigo has come back this week.
To give some history my mum has raised BP and is on medication for this but has been running high for months so they are adjusting medication to get it down. She also is on cholesterol tablets.
I’m wondering could this vertigo actually be caused by these narrow vessels? My mums mobility has never been great she is really slow and very nervous with steps etc.
If you do think it’s related what treatments can we do to relieve the dizziness. My mum has also reported feeling down lately could this be the vessels too.
Many thanks
Leslie Kernisan, MD MPH says
Vertigo (the false perception of spinning or tilting) is fairly common among older adults, but can be due to a number of different causes. The causes are often divided into the ones related to the vestibular system in the inner ear (these are called “peripheral” causes) versus causes related to the brain itself (these are called “central” causes).
It’s more common for vertigo to be due to peripheral causes, such as benign positional vertigo or vestibular neuritis. This NHS page describes some common causes of vertigo: Vertigo Causes.
It is possible for vertigo to be related to problems with blood circulation in the brain. This is called vertebrobasilar insufficiency:
Pathophysiology and Diagnosis of Vertebrobasilar Insufficiency: A Review of the Literature.
You might find it helpful to ask your mother’s doctors to explain just what type of “narrowing of the blood vessel” they saw on MRI. Are they talking about reduced circulation in the larger or medium sized arteries? Or are they referring to cerebral small vessel disease?
I would also recommend asking them to clarify what they think is the cause of your mother’s vertigo, and especially whether they think it’s peripheral, central, or perhaps a mix of both.
How to treat your mother’s feeling of dizziness really depends on what they think is the underlying cause. Many people do improve with a special form of therapy called vestibular rehabilitation. This article describes a trial of internet-based vestibular rehab, and apparently the program is available for free online at https://balance.lifeguidehealth.org
Internet-Based Vestibular Rehabilitation for Older Adults With Chronic Dizziness: A Randomized Controlled Trial in Primary Care
Last but not least, if your mother is feeling down, then I would recommend further evaluation for depression. It’s possible that her brain changes are playing a role, but regardless, if she has symptoms of depression, then she should work with her doctors to develop a treatment plan. Don’t forget to ask about non-drug ways to treat depression; depending on her situation, they can be used on their own or they can help make antidepressant treatment more likely to work.
Good luck, I hope your mom starts feeling better soon.
Pat Davis says
I am 67 years old. My MRI said chronic small vessel disease. Does chronic mean severe or could it just be mild or moderate???
Leslie Kernisan, MD MPH says
The term “chronic” has nothing to do with severity; it mainly means that the issue does not appear to be brand new (or what we sometimes call “acute”), and can be expected to persist indefinitely.
I addressed this question in one of the comments above, see here for more details.
Patty Broughton says
Hi my name is Patty. About 5 years ago i had an sudo tumor in my left eye and could not stand light lose some of my vision in the left eye. Was treated with 3 injections in the eye some of my vision returned but not all. The tumor went down and the end result was still some sensitivity to lights and still some vision lose. About 4 weeks ago i couldn’t stand to go outside or walk into an window. If is did the headaches were intense. Also the left eye drooped like i was having an stroke. Went to Dr. and they sent me for an MRI of Brain and Orbits. Also sent me back to my Eye Dr. that took care of me on the the Sudo Tumor. He was not happy they had not sent me to an Neurologist Dr. to look at the MRI due to the tumor had not returned but the blood vessels in the eye were bursting he said something more was going on the cause the problems. He started with the injection to the eye to see if that would help with some more of the vision loss. But i needed to get to the Neurologist Dr. To assess the small vessel ischemic disease they said was found. I am 59 years old , no high blood pressure, sugar, or smoke. But i do have a balance problem and seem to be very unsure of my steps. Have fallen a few times. I am very worried about having Dementia. I also seem to have the shakes in my hands so much so sometimes i have friends and family if i am ok. Why am i shaking so much. I just wants answers as to what i can do to help myself.
Leslie Kernisan, MD MPH says
It sounds like what you had a few years ago was “pseudotumor cerebri,” which is now called “Idiopathic intracranial hypertension”. I don’t know much about this condition, but apparently what is under high pressure is the cerebrospinal fluid and not necessarily the blood pressure in the blood vessels.
I took a quick look in the medical literature and in my clinical reference, and I don’t see any mention of this being associated with cerebral small vessel disease. You will have to ask the neurologists whether they think your cerebral SVD is related to your other diagnosis.
As I have said to others: I always recommend a thorough evaluation for any falls, balance, or memory problems. I would only attribute these to cerebral SVD once other causes had been checked for.
Good luck!
CAROLE says
Hi my husband has recently had a mri which showed CSVD . He’s 52 yrs old and was presenting with symptoms relative to TIA stroke.. He had aortic valve replacement surgery 2 yrs ago and is being treated for HBP which is constantly high . He suffers from balance problems and dizziness and numb sensations to his arm and face also blurred visions. His gp says nothing to worry about but we are obviously extremely concerned. He has also seen a neurologists who couldn’t find a diagnosis. We would appreciate your advice .regards
Leslie Kernisan, MD MPH says
Hm. I think you are right to be concerned, since he is having worrisome symptoms. There certainly are some people who are “medical mysteries,” but in most cases, what is needed is for the doctors to persist with a careful and thorough evaluation, even when someone is a little tricker than usual to diagnose and manage.
You may have to keep pushing the doctors to do this, by asking lots of questions, and also by looking for the most detail-oriented and best qualified specialists that you can. I’m usually not a fan of people in their late 80s or 90s seeking out such specialists (they are good at particular organs but often have trouble “seeing the forest for the trees”), but it may be quite worthwhile for someone your husband’s age.
Specific things you might ask or investigate:
– Why is his blood pressure still high? Is he on three agents for blood pressure, and has he been thoroughly assessed to figure out why his BP is so hard to control? Here is an article on resistant hypertension: Apparent and true resistant hypertension: definition, prevalence and outcomes
– What does the neurologist think is the cause of his balance problems and dizziness? Do they think it is coming from his brain tissue? His vestibular system (that’s the inner ear system that monitors balance)? Problems in the nerves of his legs and feet? All of the above? They should be able to explain what they think might be causing this. Also ask what they think is causing numb sensation to his arm and face.
– Blurred vision can be within the eyes (hence an ophthomology problem) or due to nerve and/or brain problems (hence a neurology problem). Insist that the doctors explain how they are planning to sort this out.
Obviously, it’s terrible that you have to do all this extra work, at a time when you are so worried about your husband and also probably have jobs and other responsibilities to attend to. But generally, this is the way to make sure he gets optimal evaluation and management.
I should add that sometimes doctors have actually done an adequate and thorough evaluation but still don’t have an answer, or have reached the conclusion that it’s time to wait and see how things evolve. This can be a reasonable approach (provided the initial eval was detailed and correctly done), but in this case, they should be able to explain this plan to you.
In the US, there are professional patient advocates who can be hired (usually costs money though). Some families also find it extremely helpful to connect with other similar patients in online support groups.
good luck, I hope you get some more detailed answers from your providers soon.
CAD says
I am 68, one year ago I had memory problems, however, no falling problems. Doctor ordered MRI of brain.
Results: Moderate burden of nonspecific and age-indeterminate periventricular and scattered subcortical white matter T2 prolongation. No hydrocephalus or midline shift. No abnormal extra-axial fluid collection. Basilar cisterns are open. Flow voids indicating patency are present in the major vessels at the base of brain.No hemorrhage, mass effect, or acute infarction.
Leslie Kernisan, MD MPH says
This sounds like a very “classic” radiology description for cerebral SVD. I hope your doctor has been helpful, in terms of evaluating your memory concerns and helping to maintain your brain health. At age 68 you have a better chance of benefitting from controlling any cardiovascular risk factors, compared to people who are in their 80s or older. Good luck!
Kim burgess says
Hello, I was diagnosed with CSVD two years ago at 53 following what was first thought to be a stroke however this was not the case. Lately I have been having giddy heads feeling off balance slightly my memory is getting quite bad I have days where my brain feels foggy I find it hard to concentrate, my GP feels that the CSVD is worsening I am unable to see a neurologist until the end of January 2018 as you can imagine I am worried what is your opinion is there any preventative measures I can take as no one has ever spoken about the diagnosis in any way until now.
Leslie Kernisan, MD MPH says
Sorry that you are having all these symptoms. The common sense preventive measures are essentially to try to optimize cardiovascular risk factors: blood pressure, blood sugar, cholesterol, inflammation in the body, and so forth. Exercise and making dietary changes are often helpful.
Otherwise, you need further evaluation to address two things. The first is to help you figure out what, if anything, is putting you are increased risk for these signs of small vessel damage. The other is to evaluate your symptoms of brain fog, poor balance, etc, which are non-specific and could be caused — or worsened — by any number of underlying health abnormalities. Perhaps these symptoms are related to what is causing the changes seen on your MRI, but not necessarily.
Be sure to ask a lot of questions, consider second opinions, and get a relative or friend to accompany you to the doctor, if possible, to make sure all your concerns are addressed and to take notes on what the doctors say. Good luck!
Frances Kauffman says
I was recently diagnosed with cerebral microvascular disease, my mother had passed from an aneurysm of the optic nerve, does this diagnosis increase the risks of getting an aneurysm ? I have been referred to a neurologist, have not seen him yet.
Leslie Kernisan, MD MPH says
An aneurysm is a weakened and bulging area in an artery, not in a nerve. They do happen in the brain (and elsewhere in the body) and can cause emergencies when they rupture.
Some people probably have a genetic predisposition to develop aneurysms, but it’s not clear that all aneurysms are related to genetics. I don’t know if they’ve been linked to cerebral small vessel disease. Cerebral SVD is much more common than intracranial aneurysms are.
Here is a recent scholarly article on brain aneurysms and their risk factors:
Risk Factors Associated With the Presence of Unruptured Intracranial Aneurysms
This article found that old age, high blood pressure, and smoking are risk factors. (Of course, these are risk factors for any cardiovascular disease, including cerebral small vessel disease.)
The neurologist should be able to answer your questions in greater depth. Good luck!
Venkatesan says
Dear Trish, Just now I went through your posting on CSVD problems. I am also 54 years old and I am almost having all the problems you have mentioned. Neurologists don’t give much importance to Small vessel disease. Im also having Brain shrinkage. My physical activities, sharpness all have gone. The majestic walk has faded away. Taking blood thinner and many medicines but neurologists say that there is nothing wrong in MRI. Nobody is able to judge the changes and damages done to brain. Tremors r there. Iam testing medicines one by one. Also taking Homeopathic medicines. God only knows.
Venkatesan says
I have forgotten to mention that if I skip sleep for few hours then the tinitus sound in my ear increases rapidly. All Sleep disorders persists. Is brain shrinkage responsible for all these problems?