Have you heard of Ativan (generic name lorazepam), and of the risks of benzodiazepines drugs in older adults? Is an older person you care for taking prescription medication for sleep, anxiety, or “nerves”?
Would you like an easy, practical tool to help someone stop a drug whose risks often outweigh the benefits?
If so, I have good news: a wonderful patient education tool has been created by a well-respected expert in geriatrics, Dr. Cara Tannenbaum. Best of all, a randomized trial has proved that this tool works.
As in, 62% older adults who received this tool — a brochure with a quiz followed by key information — discussed stopping the medication with a doctor or pharmacist, and 27% were successful in discontinuing their benzodiazepine. The brochure includes a handy illustrated guide on slowly and safely weaning a person off these habit-forming drugs.
This is big news because although experts widely agree that long-term benzodiazepine use should be avoided in older adults, getting doctors and patients to work together to stop has been tough. It is, after all, generally easier to start a tranquilizer than to stop it!
But through a patient education brochure, Dr. Tannenbaum’s team was able to make this tricky process much more doable for older adults, their families, and their doctors.
Why it’s important to try to stop lorazepam & other benzodiazepines
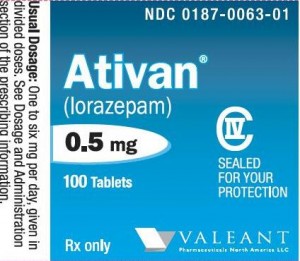
Ativan (generic name lorazepam) is a tranquilizing medication in the group called benzodiazepines (also known as “benzos”). These drugs are usually prescribed for sleep, anxiety, or agitation.
Lorazepam (brand name Ativan) is a fairly popular benzo, as the effect lasts for what is considered a “medium” length of time (the half-life is 10-20 hours).
Other benzodiazepines that are sometimes prescribed include:
- Long-acting benzos, such as Valium and Klonopin (generic names diazepam and clonazepam, respectively),
- Fast-acting tranquilizers such as Xanax (generic name alprazolam), which has historically been prescribed for panic attacks,
- Restoril (generic name temazepam), which has often been prescribed for sleep.
However, benzodiazepines are much riskier than many older adults realize. Common side effects include drowsiness and unsteadiness when walking. Research has also found that these drugs:
- Worsen balance, memory, and thinking;
- Increase the risk of falls, and of fractures;
- Can make dementia symptoms worse;
- Can easily cause physical or psychological dependency (or even addiction)
- Are linked to a higher risk of dying within a few years.
Benzodiazepines can also cause death if there is an accidental (or intentional) overdose, as high doses will slow down breathing to dangerously low levels.
Because of these problems, in 2013 the American Geriatrics Society’s Choosing Wisely list included benzodiazepines as one of the “5 Things Physicians and Patients Should Question,” when it comes to healthcare for older adults. They are also included on the Beer’s List of medications older adults should avoid or use with caution, and are at the top of my own personal list of “4 Types of Medication to Avoid if You’re Worried About Memory.”
But unfortunately, benzodiazepines are easily habit-forming, meaning that the body becomes dependent on them quite quickly. (And occasionally, some patients develop problematic abuse of these drugs.)
So it’s important to offer an older adult the right approach, and a lot of support, when it comes to getting off these drugs.
I especially recommend avoiding benzodiazepines in people with memory concerns or a dementia such as Alzheimer’s disease. Benzodiazepines act on the same brain receptors as alcohol, and they almost always keep people with dementia from thinking at their best level.
Studies have also found that people who take benzodiazepines have an increased risk of developing dementia.
For these reasons, geriatricians almost never prescribe a drug like Ativan to older adults, and we’re big fans of trying to get our older patients to taper off of benzodiazepines, whenever possible.
The must-read information brochure on Ativan and older adults
If you or your older relative is taking Ativan (generic name lorazepam) — or any type of sedative or tranquilizer — I highly recommend you read Dr. Tannenbaum’s brochure. It provides excellent information about these drugs, and includes practical tips on addressing sleep and anxiety issues without using drugs.
You can get a copy of the brochure — which includes a sample taper schedule — here: You May Be At Risk: You are Taking a Sedative-Hypnotic.
Note: It can be dangerous — as well as physically very uncomfortable — to suddenly stop benzodiazepines. Discontinuing benzodiazepines should always involve a gradual lowering of the dose. This process should always be done with the supervision and support of a healthcare professional.
Other sedatives to consider stopping
The brochure above covers Ativan along with other benzodiazepines, such as Valium, Xanax, Klonopin, and Restoril (generic names diazepam, alprazolam, clonazepam, and temazepam, respectively). It also covers commonly-used sleeping pills such as zolpidem (brand name Ambien).
Frequently asked questions about Ativan
Here are some of the questions people sometimes ask me about Ativan:
Q: Is 0.5mg of lorazepam a low dose, and is a lower dose safer?
A: 0.5mg of lorazepam is a very common dosage, and is probably the most common starter dose. The risk of side effects goes up with the dose, so yes, 0.5mg is a little safer than 1mg, and 0.25mg will be even less risky than 0.5mg.
Along with the dose of the tablet, it’s also important to consider the schedule that is prescribed. It could be prescribed just at bedtime, or sometimes it’s prescribed “as needed” two or three times per day, for anxiety (or even agitation, especially in people who have Alzheimer’s or a related dementia).
In general, the greater the total quantity of lorazepam that a person consumes every 24 hours, the greater the risks.
I’ll be honest: no matter what the dose or schedule, I consider this to be an unsafe medication for older adults, and would only recommend using it when all other alternatives have been tried first. If it must be used, it’s best to use the smallest doses that have an effect, the fewest times per day.
Q: Is it ever okay for an older adult to take a benzodiazepine?
A: Benzodiazepines, like all drugs and medical interventions, need to be considered by balancing their likely benefits with their burdens and harms.
There are some older patients — often with severe chronic anxiety — who seem to overall benefit from a low dose of these drugs.
But ideally, benzodiazepines should be used as a last resort, after making a serious attempt to treat insomnia and anxiety with non-drug approaches. These can include techniques such as cognitive-behavioral therapy, regular exercise, and stress-reduction techniques. For people with Alzheimer’s, providing caregivers with coaching on managing difficult dementia behaviors can also help.
I do have some older patients who are on benzodiazepines. I don’t like it, but usually we’ve tried other things, discussed the risks with the family, and concluded that this balance of benefits versus risks is acceptable. We also usually work to find the lowest possible dose.
Q: I can’t sleep when I don’t take Ativan. How am I supposed to get off of it?
A: It’s not always easy to taper off benzodiazepines, but research shows it’s definitely doable.
For instance, in a randomized trial to help older adults taper off benzodiazepines for insomnia, 76 older adults were assigned to one of three 10-week interventions: supervised benzodiazepine taper, cognitive-behavioral therapy for insomnia, or a combination of the two. All three groups were able to decrease their benzodiazepine use, and 63% of participants were drug-free at 7 weeks. In other words, it IS possible to learn to sleep without these medications, even if you’ve been taking them for years.
Again, if you’d like to taper off a medication such as lorazepam (brand name Ativan), please print out Dr. Tannenbaum’s brochure and bring it to your health provider, so that you can discuss tapering off together. You can find the brochure here: You May Be At Risk: You are Taking a Sedative-Hypnotic.
Q: Is it ok to use Ativan in Alzheimer’s, to manage sleep or agitation?
A: In geriatrics, we do NOT recommend using Ativan (generic name lorazepam) in people with Alzheimer’s, other forms of dementia, or any type of memory loss. That’s because it tends to make their memory and thinking even worse, and also increases the risk of falls.
Benzodiazepines also sometimes make people with cognitive impairment paradoxically agitated, by disinhibiting them. (This effect is also seen with alcohol: it can relax and quiet people, but also can make some people rowdier.)
That said, it is very common for people with Alzheimer’s to have trouble sleeping, or to sometimes become agitated and upset, and historically doctors have prescribed lorazepam or other benzodiazepine tranquilizers for these purposes. Unfortunately, this is not a safe approach. (Also unfortunate: there is basically no safe and easy way to medicate behavior problems in Alzheimer’s, as I explain in this article: 5 Types of Medication Used to Treat Difficult Dementia Behaviors.)
I’ll say it again: Ativan and other benzodiazepines should ONLY be used as a last resort, after all safer options have been exhausted.
Last but not least: I’ve found it’s more difficult to taper off benzos in people with cognitive problems. This is because to successfully taper off, the older person may have to tolerate some increased stress or difficulty sleeping in the short-term…and this can be very difficult for people who are already dealing with memory and thinking problems. (The stress of trying to taper often makes their memory and thinking worse in the short-term, even though being off benzos generally helps memory in the longer term.)
If you are caring for someone with Alzheimer’s or a related dementia, and are struggling with sleep issues, I explain options for managing this concern here: How to Manage Sleep Problems in Dementia.
Tips for aging adults & family caregivers
If you or your older loved one is taking a benzodiazepine:
- Do make sure you are properly informed about the side effects, risks, and alternative options for treating insomnia or anxiety. Dr. Tannenbaum’s brochure is a terrific resource for this.
- Do talk to the doctors about attempting a taper off the drug. It’s usually worthwhile in the long run. Even a reduction in dose can help reduce side-effects and risks.
- Don’t try to suddenly stop the benzodiazepines. Reducing these medications should be done gradually, and under medical supervision.
If your older loved one complains of insomnia or anxiety:
- Do question things if the doctor proposes a benzodiazepine or other tranquilizer as a solution. Ask for help with lifestyle changes and cognitive therapy instead. Remember that these drugs are much easier to start than they are to stop!
Here are two additional resources to help if you want to learn more about tapering benzodiazepines:
- The “Ashton Manual” is a detailed online resource, created an English psychopharmacology professor who is an expert on benzodiazepines. Find it here: Benzodiazepines: How they work and how to withdraw.
- This article describes a journalist’s experience trying to taper off benzodiazepines, and her frustrations with medical professionals who seemed to underestimate the risks of using these drugs: I Tried to Get Off Ativan.
But again, probably the most practical and usable resource for older adults is Dr. Tannenbaum’s brochure, which is specially designed to help older adults reduce their use of risky benzodiazepines such as lorazepam (brand name Ativan) and other commonly prescribed sedative/tranquilizers.
If you or someone in your family is taking this type of medication, please print it out and bring it to your doctor. Again, it’s here: You May Be At Risk: You are Taking a Sedative-Hypnotic.
Good luck making your medications safer!
This article was first published in 2014, and was significantly updated in March 2023.



TC says
I have been taking Lorazepam for a couple of months, on and off. just 1 mg. No more than that per day, and some days none at all….but now I want off of them because of all the bad stuff I have been reading. I went to the mental clinic and talked to a therapist before I started taking these pill…I was supposed to see the Dr. at the clinic..but it takes weeks to see him. So I really don’t have a prescription for them, but a friend gave me a whole bottle of hers. I never finished the bottle and now I don’t want to. I take them for anxiety and sleep problems, and they helped..but I think I can do something different to address these problems. I am 63 years old, and I am going to see the Dr. at the clinic in a couple of days… I have stopped taking them cold turkey, and having high anxiety and cannot sleep..what should I do. I have considered taking one just to get some sleep. Do you think the Dr. will help me…even though I never got a perscription for them??
Leslie Kernisan, MD MPH says
Most people find lorazepam to be very effective in reducing insomnia or anxiety symptoms in the short-term, so I’m not surprised that you found they helped. But yes, it’s generally not a good idea to rely on this type of drug, because it’s habit-forming, and creates risks and problems in the longer-term. So I think it’s good that you’ll be seeing a doctor and asking for help.
Quitting cold turkey is often uncomfortable and can potentially be dangerous. Don’t delay in going to urgent care or the emergency room if you are feeling really unwell.
You should certainly request medical help in reducing/stopping your lorazepam use and in finding better ways to manage your symptoms. Doctors are often reluctant to prescribe a controlled substance to someone who got them without a prescription, but hopefully someone will be willing to help you with this issue.
For what it’s worth, I consider 1mg to be a pretty large dose. Many older adults experience symptoms relief with 0.5mg or even 0.25mg. However when the body gets used to 1mg doses, smaller doses may provide noticeably less relief.
Good luck getting help with this medication!
Eileen says
My mother was diagnosed with cancer and put onto Diazepam at a low dose to start with. She was starting to act a bit odd after a few weeks on the diazepam she seemed to be delusional and unable to recall things from her short term memory, then she started to recall things none of the family were aware of. Mum was given a terminal diagnosed some weeks later and slowly but surely her meds increased. She was then on Oxynorm too. Mum’s behaviour was scary and we were told it was not the diazepam because that was for relaxation and she could have as much as she like as and when she liked. It was thought that it may have been the oxynorm and that because on occasion she took up to 70mg of that throughout the day/night in total, she may have been overdosing. The oxynorm was stopped dramatically but the diazepam carried on and was up to 50mg at some points, wavering around the 30mg most days but some were 40mg and some 50mg. My started to get angry and delusional about things her family were doing and not trusting us. She was accusing us of things that were not true but the medical people told us it was just the drugs adjusting. We were so frightened and scared but it all seemed to be the norm. Suddenly we were told that mum didn’t want to take diazepam any longer and as such after taking it for a good couple of months or more she was suddenly stopped it. She grew more and more agitated and angry but then occasionally she was given the odd 5 mg or 10mg to calm her down but then she would have nothing for days on end and would grow more and more delusional. Convinced we had been trying to kill her. Is it possibly that all that could be down to the diazepam? Mum had over her life time suffered depression and each time she went to the Doctor with depression the doctor gave her either valium or atavan or zanax, clonozopine or sanex and similar and every time she took them, after a few days of mixing them with her whisky she would end up trying to kill herself and delusional and even psychotic. I know she was being given alcohol with the diazepam and Oxynorm/oramorph during her terminal phase so wondered if she could have been experiencing a heightened effect of the drug when on them with alcohol and then massive withdrawal when she suddenly stopped. Thank you for taking the time to read this
Leslie Kernisan, MD MPH says
Thank you for sharing your story. It sounds like your family went through a lot of difficult and frightening times when your mother was taking these medications. (Depression in a parent is difficult, too.)
Benzodiazepines such as diazepam and lorazepam do relax many people, but they can also paradoxically agitate or confuse others, especially older adults. So I think it’s quite possible that your mother’s worsening was related to her benzodiazepines.
And then yes, even if they were making her worse, the body does become dependent on them. So suddenly stopping or reducing them usually causes significant withdrawal symptoms. In someone whose mind has been weakened, I would not be surprised if withdrawal made a person’s delusions or confusion worse. (Benzodiazepine withdrawal can also sometimes cause life-threatening stress to the heart and other organs, so these drugs should always be tapered down.)
An opiate such as morphine (in oramorph) or oxycodone (in oxynorm) does sometimes cause confusion in older adults, so it’s possible that this was contributing at times.
Honestly, it sounds like your mother had some underlying changes to the brain which made her vulnerable and prone to developing confusion and delusions. In such people, they can get mentally worse when they take mind-altering drugs, when they suddenly stop mind-altering drugs, and when they are experiencing uncontrolled pain or some other trigger for delirium.
I’m sorry you had to go through such a hard time with her. I can’t tell from your comment whether she is still alive or not. If she is, I hope the doctors have found a way to keep her feeling better. If she’s no longer with you, I wish you the best in grieving her and recovering from this experience.
Robyn says
Hi Leslie. I was prescribed Xanax about 12 years ago because I was having severe panic attacks when my son was serving overseas. I never upped my dose but eventually they stopped working as I felt worse with each day & finally traced it to the fact that I had hit tolerance on them. That is the 1st time that I researched these horrible drugs & I was shocked at what I found out, to say the least. I tried to talk to my Dr about this & she just thinks I’m being ridiculous. Anyways, for whatever reason, my last appointment with her, she informed me that she will no longer prescribe Xanax to her patients & she gave me a script for Lorazepam. I began my 1st cut at that time because she didn’t realize that they are not equivalent meds & she gave me the same amount of pills. I am desperate & determined to get off of this medication because it is greatly affecting my quality of life! It has gotten to the point that I will not do anything unless it is absolutely pressing. My relationships are suffering (except for the ones with my kids & grandkids because they are pressing) my hygiene, my job, my diet, my housekeeping (& I had OCD before this started & my house was always immaculate) my cognitive ability is awful, my memory is getting worse, my libido is nonexistent, I don’t seem to care about much, my emotions are blunted AND I experience a myriad of physical & mental symptoms from one minute to the next. Ugh!!! Sorry to rant on but I can’t seem to discuss this without my frustration getting the best of me. Anyway, I stumbled across your article & have a question about your taper schedule. I guess that I really don’t understand it. I see that it starts with a half dose on Monday, full dose on Tuesday, etc. I am currently at .5 milligrams 3 x a day. So when you are saying half dose, does that mean to only take .75 on the half days? I keep reading to reduce by .10 or .15 at a time. Any advice that you can give me would be greatly appreciated! Thanks…
Leslie Kernisan, MD MPH says
Sorry to hear you are concerned about your benzodiazepine use, but glad to see you are being proactive about addressing this.
First and foremost: I do not recommend that you or any other benzo user attempt to taper on their own. The handout is meant to provide some sensible starting guidance to an older person and their clinical team. The described taper should be suitable for most people, but it’s important to review it with someone who is in a position to consider your particular health history, and adjust the plan if necessary. Some patients do need additional psychological support or other additional clinical assistance, to keep their symptoms manageable while they taper benzodiazepines.
Now, admittedly some doctors may not have the latest knowledge of how to help patients taper their benzodiazepines. If your doctor doesn’t seem willing or able to help you address this issue, you may want to find another provider to assist you.
Regarding the taper schedule in the handout, it’s probably easiest to use when people have been taking the same dose of benzodiazepine, once a day. A clinician could help you figure out how to apply it to your situation.
Usually, benzodiazepine tapers are meant to reduce the total weekly dose by 15-25%, every 2 weeks. (This is what the taper in the handout shows.) Your current dose is 0.5 x 3 x 7 = 10.5 mg per week. So a reduction of 15% would mean taking about 9mg/week, and then in 2 weeks, your clinician would probably recommend a further reduction of 15-25%.
Some people do experience benzodiazepine withdrawal symptoms when reducing by 15-25% every 1-2 weeks. In this case, the solution is to attempt an even slower taper (i.e. reducing by a smaller percentage every 2 weeks). You can find good information and slower taper schedules in the “Ashton Manual” online: Benzodiazepines: How they work and how to withdraw.
Again, I would strongly urge you to get help from your doctor or another clinician. You can bring the handout to the visit, as it often helps clinicians to see the recommended taper schedule. Good luck!
robert says
I have been taking Lorazepam since 1982, at night or in the morning if I feel edgy .25 mg as I bite the .5 in half. I never take .5 mg in a 24 hour span. It seems to take the edge off or allow me to sleep fine. My doctor has retired and I have been forced to look elsewhere. The doctors I have encountered say I must get off it asap as it is so bad for you (I have friends that take 16 times a day what I take). I have cut down to .12 mg every second or third day. The edginess has returned along with mild headaches and if I wake up after 3 hours sleep and am up till the next night, so needless to say I am frustrated being 59 years old, being sent for random blood samples to test for drug abuse which they say is now mandatory in Canada for Ativan use. I was fine on this drug 35 years, is it really that harmful
Leslie Kernisan, MD MPH says
At 59 years old most people aren’t yet having difficulties with their memory or balance. But these issues become a concern for many older people, and it will only get harder to taper off your benzodiazepine as you get older. So although you are not taking a very big dose, it’s probably still worthwhile for you to find a way to stop using it, especially since your doctors are encouraging you to do so.
Did you read the brochure on tapering off these types of medications? (See here.) The brochure recommends a very slow taper that takes 16 weeks. You may want to ask your doctors for help implementing a similar taper.
I would also encourage you to ask your doctor for help implementing other approaches to help you with insomnia and edginess. Cognitive behavioral therapy for insomnia has an excellent track record, and is even available online through Sleepio and SHUTi. We have more information on treating insomnia here: 5 Top Causes of Sleep Problems in Seniors, & Proven Ways to Treat Insomnia.
Good luck!
Sandra Rossetti says
My drugs did turn on me after taking them for years. I kept telling my doctors and they didn’t say a thing making me be a mind reader meaning it was the pills but it wasn’t and they change you.
Sastry Addala says
My wife (73) was started on antidepressants and clonazepam 13 years ago. Ever since, she was unable to get rid of the clonazepam habit although different doctors tried to reduce/wean her away. Particularly in the past 3 years she has been suffering immensely and virtually unable/unwilling to even get out of bed. The maximum dosage that she was given at any time in the past was 1.5 mg in three divided doses. Currently we are trying 0.75mg per day but it is making her condition/suffering worse.
I have a simple question: Is it possible to reduce her suffering by increasing the dose to say, 2 or 3 mg and continue same for the rest of her life or increase it even a little more, say 4 mg after a few years? I have only one objective and that is to reduce her suffering. Kindly give your advice/comments.
Leslie Kernisan, MD MPH says
Sorry to hear of your wife’s difficulties. Unfortunately, it’s impossible for any doctor to answer your “simple question” online, you will need to work with someone in person. In particular, to answer your question a clinican would first have to review your wife’s medical history and especially understand what are the current causes of her suffering and other health difficulties. Only then would it be possible to advise regarding the dosage of her clonazepam and your other options for improving her well-being.
Now, you can probably get much better help by finding the right type of clinician. Many doctors do not have the right expertise provide your wife with the kind of help that’s likely to be a good fit.
Given the situation you describe, I would recommend you consider a consultation with a palliative-care specialist. Palliative care is a medical specialty that focuses on relieving suffering and difficult symptoms, and also emphasizes a comprehensive approach to help patients reach their most important goals.
Last but not least, you mention your objective for her but of course it’s vital to consider HER objectives for her health and wellbeing.
I hope you will be able to find a suitable clinician to help you. You can learn more about palliative care here: Get Palliative Care.
Sastry Addala says
Thank you so much for your detailed reply and advice. I will follow up on consulting a palliative care specialist here in Hyderabad, India.
kendra says
My elderly mother has been on ativan for years. We are her caretakers. She has an colostomy and has constant pain and bloating. Last time we took her in to the hospital they said she must get off her ativan and ambien for sleep. They weened her off of it and it was rough but worth it. She came home a new person that was happy and ate well and was in great spirits. 1 month later he put her back on the meds because he said it was unfair to take her off of them 🙁 she is now back right whete she started, sad and when no appetite and has continual cramping and bloating.
Leslie Kernisan, MD MPH says
Hm, this sounds odd. Sounds like someone (a doctor I presume) put your mother back on her Ativan and Ambien? Was there a reason other than “it’s unfair to take her off?” And does your mother make medical decisions for herself?
I can’t tell what happened in this particular situation, but unfortunately, it is common for doctors to push ahead without adequately discussing things with patients, unless families and patients push back and insist on further discussion before proceeding with a medication change. This is tiring and uncomfortable for patients, but right now it’s often necessary.
If you think your mother really was better off her medications, you should bring it up with the doctor or consider a second opinion. You can also ask whether a slower taper might be possible; this might be less “rough” than the first one was. Good luck!
tommy says
My father was on these for years and years .He never had to up his dose , didn’t suffer side effects and his doctor was more than happy for him to continue .My mum took nothing at all and died horribly of vascular dementia.My dad had a good death at 86 , my mother , dreadful at 90.
I think it really depends on the individual, the effects of these drugs .It was of a massive help to my father who was on 3 mg a day,and was perfectly with it ,mentally , when he passed away .
Leslie Kernisan, MD MPH says
Sorry to hear of your mother’s difficult death. Agree that it does depend on the individual. However initially as clinicians — and even as patients — we can’t tell how an individual will respond over the long term, so we should start by working with what we know from observing groups.
(For instance, we all know people who smoked regularly and lived to their 90s, but they are exceptional. If someone is 40 and smoking, we cannot tell if they will be among the exceptional ones or not, although better analysis of genes and cellular activity might enable this soon.)
For benzodiazepines, my experience has been that most patients and families have been told very little about the downsides, and they haven’t been encouraged to consider alternatives. Ideally, people would be better informed before proceeding, or continuing on these drugs.
I will say that in some cases, the benefits seem to outweigh the risks. So I don’t want to say it’s *never* reasonable for older adults to take benzodiazepines. But given that they increase fall risk and worsen thinking, it’s worth thinking carefully before continuing with them long-term.
Carol says
I take two of the benzo’s for sleep; one for restless leg syndrome and one for insomnia per a sleep specialist that gives me the prescriptions. I’ve noticed the Temazepam seems to cause memory loss and I’m concerned…very concerned. I’ve been on these two drugs for a long time (4 years at least). Thanks for the schedule to discontinue them. I’m in my early 70’s and don’t want to take them anymore. I will talk to the sleep doctor too and tell her of my desire to quit them. I also use the lowest dose of the hormone patch and now I’m concerned about that too.
Leslie Kernisan, MD MPH says
Great that you are being proactive about this. If you are concerned about your memory then I would definitely encourage you to discuss your concerns with your doctors. It is often possible to taper off benzodiazepines, but this should only be done under medical supervision. Good luck!
Anonymous says
I am so impressed with the information you are providing. I am 60 yrs old & have been taking lorazepam for over 13 years. My doctor has me take hydroxyzine as well. It is for sleep. My memory has been impaired and I am eager to get off both medications to stop the harm to my brain. Thank you Dr Kernisan for addressing this problem.
PS I must admit it was a relief to have something to ensure I would sleep but the memory loss is motivating me to try and get off the sleep cocktail. Thank you.
Leslie Kernisan, MD MPH says
Thank you for sharing your story! I’m glad the information is helpful, and great that you’ve decided to work on this issue.
Your situation unfortunately is not uncommon. People often start medications for sleep when they are going through a stressful period in mid-life, and then their doctors never quite get around to revisiting the issue. However if you tell your doctors of your concerns and ask for help in stopping or at least minimizing these medications, they should be able to assist you.
Also, I’m sorry to say there are usually no easy and fast ways to learn to sleep without these medications. That said, with enough coaching and help many people do learn to sleep without medications. Often therapy helps — such as cognitive behavioral therapy — as well as incorporating relaxation techniques and exercise. (Note that exercise may mainly help sleep only after one has stuck with it for a few months.)
For more ideas on how to handle insomnia without drugs, try reading something like The Insomnia Workbook (you might find it at your public library). It’s written by a sleep medicine psychologist and has lots of good ideas.
Good luck! Getting off sleep medication takes time and persistence, but for most people it’s good for health in the long run.
Brenda says
I cared for a lovely little old lady [ think she was 96] who just loved getting her blue pill at night time. She gave a beautiful smile as she took it, and would hold my hand and say “thank you dear, now I get to have wonderful dreams and forget this life”
So it does have its place, for the right person .
Agree with all stated in the blog tho for those who haven’t had 96 candles on their birthday cake
Leslie Kernisan, MD MPH says
Thanks for sharing this sweet story. I, too, have found that many older adults love their benzodiazepine. (Heck, I’ve met people of all ages who are fond of this line of medication; almost everyone appreciates a little relaxation.)
As I say in the post, I think the key is to realize that these medications do come with risks and side-effects, so it’s important to be informed and consider alternatives.
But it’s certainly possible to weigh the benefits and risks, and then decide to continue the medication.
larry says
Please help me
Leslie Kernisan, MD MPH says
Unfortunately, it’s not possible to provide much help online, beyond providing useful resources and perhaps suggesting some questions to ask your usual doctors. If you are concerned about benzodiazepine use, I recommend printing a copy of Dr. Tannenbaum’s brochure and discussing it with your usual health provider. Good luck!
(And of course, in case of emergency or severe symptoms, go to the nearest emergency room or call 911.)
Sandra Rossetti says
Thank you, but the ER’s won’t do a thing
Sandra Rossetti says
Risks!!! I have been on a living hell of a life I’m finding out now from being on 3 different kinds of “benzo” through the years. I had a specific problem about 30 years ago, doctor gave me Xanax, then Klonopin, now Ativan the worse. Thru the years I could not breathe, gave me different anti depressants which I am now thinking the benzo were the reason. I am now so sick wonder everyday if Im going to die. When I go to bed at bad times I leave notes good bye notes for my kids. I broke down in my doctor’s office today – he would not give me anything more. Finally he said I could take Zoloft which has terrible side effects for me – I’ve tried it many times. He would not take me off the Ativan and in there I was so upset I forgot to pursue it. Scared…..
Leslie Kernisan, MD MPH says
Sorry to hear of this, it does indeed sound difficult. If you think you would benefit from being on less or no benzos, please keep trying to bring this up with your health providers. Sometimes it helps to bring in a trusted family member or friend to help you advocate for working on this. Good luck!
Sandra Rossetti says
Thank you for this article. No one around here seems to know how to help. Now the dr has me taking 23 ml of Viseral, I’m so sick and can’t seem to relax. Taking very small am’ts of Ativan. Don’t know where else I can go for help. Do you. Can you help. Is it possible to go to a rehab or ? Will I ever be okay. Drowsy, dizzy, sick to my stomach.
Leslie Kernisan, MD MPH says
Sorry but I can’t help. You will need to find local providers to assist you. You could also try contacting a community hospital or community clinic; they are sometimes more aware of local options for rehab or tapering addictive substances. You may also want to ask a family member or trusted friend to help you research your local options. Good luck!
Mitch says
Ativan is one of the worst to quit. I got 37 years never missing a day…… never missing a 8-hour block. Got off methadone in 60 days. Methadone withdrawal is a cup cake party compared to benzos and most say methadone is for life. Not true. The half life is the magic secret-and same goes for benzos. It’s all over the web so I won’t elaborate.
Furthermore do NOT read or buy into the horror stories you see online. Many of those fools couldn’t climb out of a paper bag and proof is me and methadone. According to most addicts you will go to hell and back,, lol it’s 100% BS!!! That is unless you buy the story. Don’t buy it- you are different. Unique. You don’t know these folks background. Perhaps they have underlying mental issues? No success in life whatsoever (I know one of these). Or are just plain weak souls.
I’m going on Valium and I expect to do it using positive mindset. Refocus that withdrawal energy into something positive…. the lower the low the higher the high once clean. I’ve been having interdosal withdraws now for 2 years & never recognized it. Now I do.
Also-ask for a beta blocker for pounding chest and head tension. I take atenolol when I’m quitting. Be ready to die (metaphorically speaking). Do anything and everything necessary. Prolly have to take leave of absence for 30-60 days.
My point is: make it priority! I’m relaying all I know from Methadone detox and intend to blow thru Ativan detox ASAP. Bring on the pain. Embrace it and you will become a new person. Fight it, complain, self loathe and sure….. you too will be going to hell and back. You not need to I promise. CBD oil is beneficial and easy to get albeit pricey. I know I’m in Colorado. Pure cbd doesn’t show on drug tests. Again- done 3 fine and one I failed. Now I do a pre test at home before giving my UA to a facility. KNOW what your going to pee B4 ever giving a UA. DG sells tests for $1/ea.
Best of luck to all battling this. Sincerely MB. Boulder,CO
Ann Balthaser says
Hi Sandra
My daughter (52) is going thru this. Says she feels like she’s out of her body and in a dream. It’s a living hell and I feel so helpless.
Sandra Rossetti says
Thank you but be careful of Methadone. My son got addicted to opiates and has gained tons of weight. He doesn’t look like the same person and now he’s got diabetes all because her was treated and retreated for back pain.
JoMarie Indovina says
It is a living hell.
Leslie Kernisan, MD MPH says
Dizziness can be caused by many things. I would recommend being evaluated by a medical professional.