In this post — the last in a 4-part series on better planning for health crises and end-of-life care — I want to tell you about a document that I wish more families knew about: POLST.
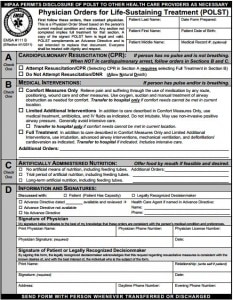
POLST (which stands for Physician Orders for Life-Sustaining Treatment) is a legal document meant to tell healthcare professionals what you want done, in the event of a medical emergency. It’s kind of like a pre-hospital DNR (do-not-resuscitate), but much much better. (For starters, you don’t have to be DNR to use a POLST form.)
Note that POLST is not an advance directive, although when doctors ask if there is an advance directive, they are often thinking of POLST as well. (Because what they are really asking is, is there any pre-existing documentation that can help us understand what we should and shouldn’t do?)
And it’s not a perfect approach to making sure older adults get the care they want and need, when a health crisis hits. If you have heard of POLST, you may very well have heard some negative things; I’ve certainly heard some complaints over the years about POLST forms, or about how something didn’t quite work out despite the presence of a POLST.
Still, I really like POLST, and discuss POLST forms with many of the older adults and families that I work with. In California, POLST has largely replaced the pre-hospital DNR forms that some older adults used to have.
Furthermore, a study published in 2014 confirmed that in Oregon, where the POLST approach was first pioneered, POLST forms have helped get end-of-life wishes honored more often. (The New Old Age Blog published a related post recently, titled “When Advance Directives Are Ignored.”)
If you’re caring for a frail older person and you live in one of the many states with a POLST program — click here to find out if your state has POLST — I highly recommend you incorporate this tool into your loved one’s advance care planning. In most cases, a surrogate medical decision-maker can complete a POLST form.
In this post, I’ll share some resources on learning to use POLST to better plan for health crises and end-of-life care.
I’ll also offer some tips on avoiding common pitfalls, such as completing POLST without first addressing the learning and conversing parts of advance care planning.
Note: Some states have chosen a different name when they implement POLST. Alternative names include MOLST (Medical Orders for Life-Sustaining Care), MOST (Medical Orders for Scope of Treatment), or POST (Physician Orders for Scope of Treatment).
Useful Resources About POLST
Here are some useful links for older adults and family caregivers:
- POLST.org: This site explains the “POLST paradigm.” It includes a section for patients and families, and also has resources for professionals who might want to develop POLST in their own state. It does not have a sample POLST form, because those have to be developed by each state individually. If you want to find out if your state has a POLST program, or is planning a POLST program, be sure to check the state directory feature.
- POLST California: This site is most useful for older adults and families in California, but the basic information about POLST is well-written and should be useful to people from other states. I like that it’s easy to view the actual POLST form (click the link in the lower part of the main home page). I also like their printable POLST guides, which are available in English, Spanish, and Chinese.
-
“POLST: An improvement over traditional advance directives”: For those who enjoy a more in-depth resource, this is a scholarly article written to explain POLST to healthcare professionals. It seems to be freely available to the public and does a very nice job of explaining how POLST compares to traditional advance directives. I especially like that the author (a geriatrician) emphasizes the need for shared, informed medical decision-making as part of the POLST process.
- “A Final Prescription“: This is a 2010 New Old Age Blog post describing POLST. It provides some good examples of situations in which POLST can help aging adults facing a health crisis.
Common POLST pitfalls, and how to avoid them
Here are some of the problems that I’ve seen occur with POLST, and how you might be able to avoid them.
Bear in mind that POLST is developed and regulated by each state individually, and that most POLST programs are relatively new to those states that have them. (California’s POLST was first implemented in 2009.) So, some of these problems are undoubtedly related to “growing pains” in implementing POLST, or even in skillfully addressing end-of-life issues with patients and families.
- Pitfall: Signing POLST without adequate conversation and input from clinicians.
I’ve seen this happen in a variety of ways. Sometimes it’s because a residential facility strongly encourages a family to complete a POLST, but they don’t help arrange for the older adult and family to discuss with a suitable clinician. In other cases, I’ve heard of families asking their primary care doctors about POLST, only to be given the form and told to complete it on their own. (Unlike an advance directive, POLST must be signed by a healthcare professional.)
How to avoid: Insist on having a conversation with a qualified clinician, before signing a POLST form. A good approach is to review the basics of advance care planning first (see below). That way you’ll be better prepared to discuss with the doctors. If your doctor is unwilling to discuss POLST, or is struggling to help you with advance care planning, try to find a clinician trained to discuss end-of-life planning, such as a geriatrician or palliative care doctor.
For the basics on advance care planning, see this post. You can also review my Slideshare presentation below. Like an advance directive, a POLST will best serve you if it’s completed after you’ve gone through a process of education (what is the health situation? what crises are likely to come up?), reflection (what are my loved one’s values and preferences?), and conversation (have I discussed with my family? with the doctors?).
If you or your loved one did sign a POLST, and you later realize there wasn’t much conversation beforehand, don’t forget that it is always ok to ask doctors to review and discuss a previously signed POLST. This will help you and the doctors work together better, and it’s usually easy to complete another POLST if revisions are needed.
- Pitfall: Not being able to find POLST at the key moment.
A key feature of POLST is that it’s supposed to “follow the patient” as he or she moves from one place of care to another. So for instance, if an older person has a POLST in a nursing home and there’s an emergency, the paramedics are supposed to bring the POLST to the emergency room. Of course, this doesn’t always happen the way it should, so it’s not uncommon for families to discover that hospital staff haven’t actually reviewed a person’s most recent POLST.
How to avoid: This problem reflects the fact that our healthcare system is often bad at having up-to-date information at the point of care. This is unfair to patients and families, but unless you live in a state that has a well-functioning system for sharing advance directives and other key information, you will probably need to be proactive about making sure doctors review the latest POLST form when a crisis hits.
Some states have created an online registry for POLST forms; my understanding is that these currently exist in Oregon, West Virginia, and New York.
But even if a state registry is available, it’s always a good idea to be prepared to bring a copy of POLST and other important documents in person, should there be an emergency event.
If you are technology-inclined, you can also look into one of the new apps or cloud-services that promise to keep your important documents secure and handy. I have also seen families keep a copy of POLST and other key documents in less secure cloud storage spaces (such as Google Drive, or Evernote, or even their email accounts). This is risky in that regular cloud storage is not as well protected as storage designed for health information, but I certainly can understand that people often opt to use a service they are already familiar with.
What’s most risky of all is to assume that your loved one’s POLST will be easily available to doctors during an emergency. It should be but it often isn’t, so I encourage family caregivers to be proactive about keeping a copy of POLST on hand, and making sure their loved one’s healthcare providers are aware of the contents.
- Pitfall: Not revising POLST after health situation gets better (or worse).
Here’s a situation I’ve encountered a few times in the past year: a frail older person is hospitalized, seems to be doing poorly, and so during the hospitalization the family meets with the doctors and then completes a POLST indicating “Comfort Measures Only.” For many of those older patients, this remains a good fit for their preferences and situation. But some older patients actually make a significant improvement during the 6-12 months after hospitalization. Yet no one revises their POLST, so when an illness requiring possible hospitalization comes up, people are confused and uncertain as to what to do.
This situation illustrates why it’s important to treat advance care planning as an ongoing process. A medical care plan often needs to be updated as a person’s health, situation, and preferences evolve. Although older adults often experience a decline in health over time, it’s not uncommon for many of them to slowly improve, especially if they have a supportive living environment with lots of TLC (tender loving care, which I try to “prescribe” whenever possible).
How to avoid: Try to remember to review POLST and other advance care planning documents regularly, especially after a new diagnosis or major change in health status.
I myself like to set a date to reassess an older person’s situation, preferences, and care plan. This is especially helpful after hospitalization, since it can be easy to forget to re-address POLST in an older person who is doing relatively well. (Whereas repeated hospitalizations tend to get everyone’s attention; they are also a good opportunity to review POLST forms.)
What experience have you had with POLST, or POLST-like documents?
Have you had any experience with POLST, for yourself or for an older loved one? Do you have any questions regarding POLST, or advance care planning for older adults?
Can you recommend any resources that have been helpful to you?
If so, I’d love to hear from you in the comments section below.
Also, if you’d be interested in getting more practical geriatrics health information delivered to your email inbox, click here.



Jennifer McKenzie, MSW says
As a point of reference, I am a medical social worker and I provide counsel to people admitting to hospice care as a part of my daily duties as a team clinician. I wanted to add to this topic that having part A marked DNR and having Full Treatment marked in Part B seems inconsistent to our team. Since it is not infrequent to see this on admitting patients, we make it a priority to engage the patient and family for clarity on their wishes.
I will also note that some patients worry that if they sign a POLST with DNR/CMO that their hospital system care will see this as license to “write [them] off” and not provide the care they are afforded.
Nicole Didyk, MD says
Thanks for sharing you experience. I can understand the perception that those two preferences on a POLST form would seem inconsistent, and I’m glad to hear that it promotes a more detailed discussion about advance care wishes.
I’ve also had the experience that some feel a “DNR” could lead to less attention from the medical team, and to be honest, there may be some grounds for this fear in some cases. We have a long way to go to educate everyone about person-centered care and palliative care for things other than end of life.
Thanks for the work that you do and for taking the time to comment!
Monika says
I am seeking proper guidance on behalf of my mother currently in ICU who is cognitively impaired (dementia/non-verbal). I have legal power of attorney and an advance care directive allowing me to be the decision maker for my mother if she cannot do so for herself.
A POLST was completed 6 years ago (April 2014). It was signed by a physician (who did not know my mother and was not familiar with her medical history), a social worker completed the form, and it was signed by my mother while at a skilled nursing facility for a short period of time. I was not present when the POLST was presented to my mother and completed. My mother, about six months prior, was diagnosed with mixed dementia. In 2014, and at this time, my mother was not considered to be at risk for a life threatening clinical event because of a serious life limiting medical condition or advanced frailty. She was doing well enough and was at the skilled nursing facility for IV antibiotics.
In November 2013, with this diagnosis of mixed dementia, my mother had notarized a power of attorney and advance care directive appointing me as her surrogate.
I’ve read information that the POLST can be changed or voided by a health care professional, a patient with capacity (my mother does not have the capacity now), or the patient’s surrogate if the patient lacks capacity. I wish to void/revoke the old POLST dated in April of 2014 on file at this hospital and/or complete a new POLST based on what my mother’s wishes would be now that she has advanced frailty (and other medical conditions that have placed her in the hospital in ICU which are still not life threatening).
The POLST was not reviewed with me, in more recent years, with my mother’s health declining and her being admitted and discharged from this hospital over the past two years. I do not have the original copy. A copy was presented to me in February of 2020 when my mother fell ill again and was also in ICU.
My mother wants to live but she cannot verbally express herself. She has appointed me to make these decisions on her behalf, which will be in her best interest and based on her advance care directive. I want my mother to live also. This is my mother who I love very, very, very, very much!
Can you please offer guidance on what I need to do to void, revoke, change the POLST so that my mother will receive all the care and life sustaining treatments available to her which she deserves and should be entitled to which she is not receiving now. Thank you very much!
Nicole Didyk, MD says
I’m so sorry to hear that your mother isn’t well. I’m not a lawyer, and my practice is in Canada, but I can share the advice I would give to someone in a situation similar to yours.
My understanding of a POLST is that it is primarily used in an emergency to determine the initial level of action to take. For example, if a POLST indicated that a person wanted to go to hospital, but not be in the ICU, then chances are they would not end up in a ICU. It’s unusual, at least where I practice, to be in an ICU and not be receiving intense medical care.
However, not everyone who is in an ICU setting is likely to benefit from the type of care that is being offered there. It’s common, regardless of a POLST or advance directive, to review progress and prognosis, and talk to families about the goals of the person, and whether another treatment plan would be more appropriate.
A Substitute Decision Maker, who usually also a Power of Attorney for health care, would be called upon to make decisions if a person isn’t able to speak for themselves, and would do so based on all of the information from the medical team, and knowing the person’s (not the Substitute Decision Maker’s) prior wishes. At this stage, a POLST can be used as a reference, along with other information.
If a Substitute Decision Maker feels strongly that the preferences of the individual have changed significantly, then this should be discussed with the health care team, but seeking to revoke the POLST may not be a good use of time and energy, as it is more for emergency situations and less relevant in ongoing hospital care.
Sam Capra says
Thank you Dr. Didyk. My physician feels selecting DNR in Section A and Full treatment (trial period) in Section B is confusing and incompatible. In A you are assumed to have no pulse and not breathing so basically you are dead and in section B you are not dead so I don’t understand why there would be any confusion or incompatibility. I agree with you.
Sam Capra says
Can you select no CPR in Section A of POLST and trial period of full treatment in Section B or would this be too confusing?
Nicole Didyk, MD says
I think you can select trial of full treatment in section B and still want to be a “DNR” in section A. Essentially, the medical team would provide full care if the person appeared to have signs of life (pulse, breathing), but if the person appears to have no vital signs, they would not intervene.
Gail Mc Donald says
I currently have diabetes and am 71 years old. My doctor gave me a POLST form to complete. My most recent physical revealed I am in excellent health and my lab numbers are good as well. Was I given this form due to my age or the fact I have diabetes B or both? Just curious why I received it when I have much older friends who are in poor health who are unaware of this form. thanks for any input
Leslie Kernisan, MD MPH says
Hm, interesting! Most experts recommend that POLST be discussed and completed when people have advanced serious illnesses, significant frailty, or other signs of limited life-expectancy. One rule of thumb would be if the health provider would not be surprised if a person died within a year.
If you are 71, have diabetes or a few other chronic illnesses, but are generally in good health with good function and infrequent hospitalizations, I would not say you meet the criteria for “advanced serious illness”, frailty, or limited life-expectancy.
I am guessing that your provider is either unaware that POLST is recommended for people who have worse health than you, or perhaps your provider just thinks POLST is good for all older adults. It might be good to have a conversation with your provider about this.
I do recommend advance planning with a healthcare directive, and would especially recommend PrepareforYourCare.org’s easy advance directives, you can learn more here: End of Life Planning Made Easy Through PREPARE.
Your older friends in poor health would ideally do an advance directive (again, I recommend PREPARE, it’s great), and also consider a POLST. Good luck!
Betty says
So glad I had this doc when the EMTs were called for my 96 yo father. They were looking to each other as to what to do, is when I realized I needed to go to the fridge & take them Dad’s prep’d POLST. Not sure what would’ve transpired if I hadn’t. So since then I had wondered whether I need to do this myself. But this page made me realize maybe I ought to just do the Advance Health Care Directive instead. Regardless of one’s age, think to have a clearer idea of an individual’s desires during a moment of crisis is critical. TY
Leslie Kernisan, MD MPH says
Thank you for sharing this comment and your father’s story. How fortunate that your family had prepared and also that you were able to help the EMTs find the POLST.
In terms of whether you should do it, POLST is usually recommended for people who have significant chronic illness or frailty, because they are more likely to have a serious emergency (and are less likely to recover from aggressive life-sustaining interventions). Otherwise, the main thing that is recommended is advance care planning and completion of an advance directive.
For that, my current favorite resource is PrepareForYourCare.org, which offers a step-by-step process to help older adults reflect on their preferences, and also now includes easy-to-use advance directives for all 50 states.
Good luck!
VH says
Our Texas Out of Hospital DNR form is quite vague.
Does a physician really have to sign the form if the patient is mentally competent?
And does the OOHDNR prevent electrical synchronized cardioversion for unstable tachycardia?
Leslie Kernisan, MD MPH says
I am not familiar with the Texas form, but it appears the Texas Department of State Health Services provides a copy with some guidance:
https://www.dshs.texas.gov/emstraumasystems/dnr.shtm#form
Based on this, it seems to me that patient can sign on his/her own, if mentally competent, but there need to be witnesses or a notary.
In California, the DNR section of POLST refers to situations in which a person has no pulse and/or isn’t breathing.
Texas seems to be in the process of setting up a “Medical Orders for Scope of Treatment” form, there is info here: http://www.northtexasrespectingchoices.com/m-o-s-t/
I would recommend you ask a Texas physician — perhaps one with experience in end-of-life care — about handling advance directives and potential DNR orders for someone who might want cardioversion for unstable tachycardia.
Victoria Wolf says
I am a professional and fill out POLSTs everyday and the one thing I keep bumping up against is Part A patient wants DNR… Part B they want trial period of resuscitation. MDs do not want to sign it because they feel it is incongruent. It is my understanding that a person can be both DNR if found at home, but once in ED or hospital can have the trial of full code. What am I missing. And, to whom is Part B directed….hospital or outside of hospital situation??? Thanks.
Leslie Kernisan, MD MPH says
Hm, interesting question.
Full treatment, as I understand it, essentially refers to ICU-level care, and various types of “life-support” (e.g. intubation, mechanical ventilation, temporary dialysis, etc.)
I agree that people can choose to be DNR and still want full treatment in the hospital. It does strike me as an unusual choice, but that might be because I do most of my POLSTs with people who are already declining and have limited life expectancy.
Part B is less about “in hospital” versus “out”, and more about what should be done in the event of very serious illness. If a person is full treatment, they will need to go to the hospital. For selective treatment, it will depend on the severity of the situation and whether the person expressed a desire to avoid hospitalization if possible. For comfort-focused, hospitalization should only be used if needed to control symptoms. So Part B provides guidance as to when hospitalization should be considered.
For more on understanding POLST, there are some good clarifications here: POLST QUICK REFERENCE FOR PHYSICIANS. This could even be printed and given to the physicians you are working with, since there’s a section on addressing “No CPR And Full Treatment Rationale.”
Victoria Wolf says
Thank you for replying. My experience everyday with the Selective Interventions in Part B is this, patient comes to the ED, POLST is looked at, MD sees DNR part A, SI checked in Part B. This SI provides them the go ahead to begin any testing in the ED. I have never heard of EMTs upon seeing the SI checked asking the question to patient or families “depend on the severity of the situation and whether a person expressed a desire to avoid hospitalization if possible”. EMTs ALWAYS bring them in, even for CMO POLSTs, (maybe not if patient is already on hospice, but even then they often bring them)they want the ED to decide….seems like a concern for liability. Studies are started and DPOHC attempted to get in touch with for decision making if patient cannot. The POLST to MDs often is confusing in the ED setting when A and B are different from each other. As a Palliative Care nurse I try to help them as best I can when figuring out patients wishes in emergencies, it can be harrowing for all. Most Doctors are not comfortable until they hear directly from family, and in situations of sepsis and respiratory emergencies when patient are declining rapidly, further discussion is absolutely needed even if POLST says DNR…. DNR, as you said in CA, is only if heart and breathing has stopped. There are a myriad of things that can and do happen in between that the POLST saying DNR can not address. Sometimes it is only the beginning and gives only an inkling of what patient and family lean towards. It is absolutely better than nothing, and hopefully starts conversations between family members. But I know some of the Doctors in the ED struggle with them. I would like to see continued work on defining the POLST and education of it for all medical personel. Thanks again
Leslie Kernisan, MD MPH says
Thanks for your comment. Yes, I agree that the issues you describe are common, so there is still a ways to go, when it comes to using POLST to really provide patients and families with the right care at the right time. Still, as you say it’s better than nothing, and also I know that various expert groups are working to use what we’ve learned from POLST so far, to improve the paradigm and the related processes. So hopefully we’ll see improvements and progress soon.
James Leonard Park says
I am working on a replacement for POLST.
Here is my current list of problems:
http://www.tc.umn.edu/~parkx032/POLST.html
Here is my current draft of the replacement, ELMO:
http://www.tc.umn.edu/~parkx032/ELMO.html
Leslie Kernisan, MD MPH says
Great that you are trying to improve things. You may want to connect with your state’s POLST working group, and with experts who are working to improve advance care planning documentation. Good luck!
Gerald Roux says
My wife and I are 84 and asked our GP about POLST. He gave us two forms and said to fill them out. We did and returned them to him. He signed them. We had no discussions with him regarding the POLST. We have added the forms to our end of life paperwork and have discussed them with our family.
Thank you for your informative and needed posts.
Leslie Kernisan, MD MPH says
Thank you for sharing this story. I’m sorry to hear your doctor didn’t offer more input and guidance. Discussing a POLST form offers a good opportunity for a patient and doctor to come to a better understanding, which often means the doctor can provide care that’s a better fit for a patient’s needs and preferences. However, a thoughtful conversation takes time, which is often in short supply in primary care.
If you have any questions or concerns, you could try scheduling a visit just for the purpose of reviewing your advance care planning, including the POLST forms.
I’m glad to hear you’ve discussed your planning with your family. Thanks again for this comment.