
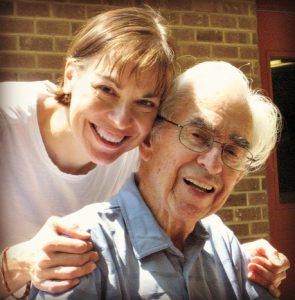
When is the last time you had a really meaningful conversation with someone from a different generation? And who was it with?
Was it with a grandchild? A niece? Your own parent? A neighbor? Or maybe even the person standing next to you in line at the store?
While these types of connections happen every day across the United States, they probably aren’t happening enough.
And that’s a shame, given that research suggests these intergenerational connections are actually really valuable to people of all ages.
For instance, in 2018, the AARP conducted a national survey of grandparents to learn more about this intergenerational relationship and what it means to older adults. Almost 90% of grandparents reported their relationship with their grandchildren is good for their mental well-being.
However, the survey also found that distance was the number one barrier to seeing grandchildren more often, with over half of grandparents reporting they have at least one grandchild who lives more than 200 miles away. Sixty-one percent of grandparents reported wanting more information about connecting with their grandchildren and staying relevant in their lives.
I first heard about these findings at a conference last summer, when I met Kerry Byrne, PhD, a fellow aging and family caregiving expert who has developed a special interest in intergenerational connections, and in the grandparent-grandchild relationship in particular.
Partly due to her own experience living abroad and trying to keep her children close to their grandparents, in 2019 she founded The Long Distance Grandparent, a website dedicated to helping grandparents and grandchildren connected, even if they live far from each other.
I find this topic of intergenerational connections fascinating. Among other things, it has a role in countering ageism!
So I invited Kerry to join me on the podcast, to talk about how older adults can stay more connected to people of different generations, whether that’s with grandchildren or with people outside their family.
If you are a grandparent yourself, or just want to learn more about why intergeneration connections matter and how you can foster them in your own life, I hope you’ll take a listen to the podcast, or read through the transcript.
Both are available on the show notes page, which you can find here: 102 – Interview: The Importance of Grandparents & Intergenerational Connections
5 Practical Ways to Have More Intergenerational Connections
Here are five specific things Kerry suggests that older adults can do, to foster more intergenerational connections:
[Read more…]




 You’ve likely already heard the news: the flu is pretty bad this year, with the Centers for Disease Control (CDC)
You’ve likely already heard the news: the flu is pretty bad this year, with the Centers for Disease Control (CDC) 


