This is the fourth in a series of posts covering the Healthy Aging Checklist.
Again, the Healthy Aging Checklist summarizes the six fundamental activities I recommend when asked what to do to maintain the best possible health while aging. They are:
- Promote brain health and emotional well-being.
- Promote physical health.
- Check for and address common aging health problems (such as falls, memory concerns, depression, incontinence, pain, isolation, polypharmacy).
- Learn to optimize the management of any chronic conditions.
- Get recommended preventive health services for older adults.
- Address medical, legal, and financial advance care planning.
In this post, I’ll cover the fourth item: learning to optimize the management of any chronic conditions.
Now, people are often very interested in “prevention” and in “staying healthy.” But far fewer people seem to be interested in making sure that they and their doctors are doing the right things for any chronic conditions they already have, and — equally importantly — avoiding the wrong things.
This is a serious oversight, because most of the “aging” problems that older adults eventually develop are due to chronic health conditions that have progressed or caused complications.
So optimizing the care of chronic conditions is very important for the prevention of future health deterioration. And it’s also vital to helping older adults feel and function their best in the here and now.
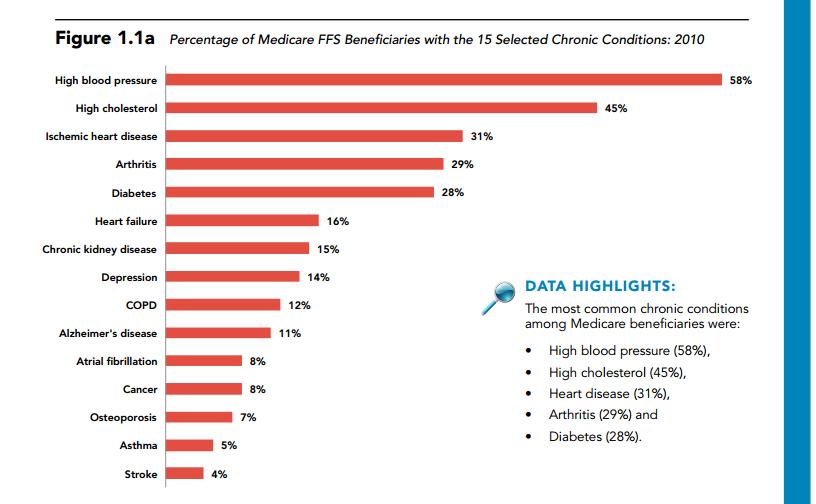
According to Medicare, over two-thirds of beneficiaries have two or more chronic conditions. Here’s a figure from the Medicare Chronic Conditions Chartbook, showing what percentage of older adults are affected by the 15 most common chronic conditions:
I can’t emphasize this enough: these chronic conditions often are the key drivers, when it comes to an older person’s symptoms, health crises, health declines, and the eventual development of disabilities.
Furthermore, I’m sorry to say this but here goes: you should not assume that doctors will provide you with optimal care for chronic conditions. Experts have estimated that patients get only about half of recommended healthcare. A large body of healthcare quality research has repeatedly documented that it is very common for older adults to receive healthcare that varies from “wrong” (e.g. totally counter to guidelines with no documented justification for this) to “sub-optimal” (which means it’s not very deficient but could and should be better).
Later in this article, I will go into more detail on why doctors often provide sub-optimal care, and what you can do about it.
But first, let’s review what’s at stake and why it’s worthwhile to make sure you optimize the healthcare of an older adult’s chronic conditions. I’ll then finish by providing some practical tips to help you be proactive so you can optimize the care of chronic conditions, for healthier aging.